5174
Fat Saturation in Musculoskeletal MRI using Spectral Heterogeneity Adaptive RF Pulses (SHARP)1Siemens Healthineers, Rochester, MN, United States, 2Mayo Clinic, Rochester, MN, United States, 3Siemens Healthineers, Macquarie Park, Australia, 4Siemens Healthineers, Austin, TX, United States, 5Siemens Healthineers, Portland, OR, United States
Synopsis
In this work we propose the use of adaptive RF pulses for achieving uniform fat-saturation (fat-sat) that is robust to B0 and B1 heterogeneity often observed in musculoskeletal MRI. A prototype with Spectral Heterogeneity Adaptive RF Pulses (SHARP) was developed to improve the quality and functionality of fat-sat. SHARP was shown to provide fat-sat with higher robustness to B0 and B1 heterogeneity compared to SPIR and SPAIR fat-sat methodologies.
Purpose
Hyper intense signal from fat in MRI may obscure pathology such as inflammation or edema. Fat is suppressed in MRI using the chemical-shift and/or the difference in the T1 values between water and fat protons (1,2). Hybrid approaches such as spectral pre-saturation with inversion recovery (SPIR) and spectral attenuated inversion recovery (SPAIR) use both the chemical-shift and T1 differences between water and fat protons for fat suppression. SPIR is susceptible to main magnetic-field (B0) and transmit magnetic-field (B1) inhomogeneity (1). SPAIR is robust to B1 variation due to the use of adiabatic pulses (1). However, SPAIR is sensitive to B0 heterogeneity (1).
In this work we propose the use of adaptive RF pulses for achieving uniform fat-saturation that is robust to B0 and B1 heterogeneity often observed in musculoskeletal MRI.
Methods
A prototype for achieving uniform fat-saturation (fat-sat) with Spectral Heterogeneity Adaptive RF Pulses (SHARP) was developed with functionality to change fat-sat RF pulse type, offset, bandwidth, time-bandwidth-product (TBWP) and flip-angle. Fat-suppression was performed by selectively exciting the fat protons and saturating the fat-signal using dephasing gradients. In order to improve B0 homogeneity a second order shim was used. Fat spectrum has multiple peaks that can be observed at chemical-shift frequencies of −3.3 ppm, −2.5 ppm, +0.7 ppm, −3.7 ppm, −1.8 ppm and −0.4 ppm relative to water (peaks are listed in order of their relative percentage contribution to the fat signal (3) ). At 3T, the fat peaks are at −420 Hz, −318 Hz, +94 Hz, −472 Hz, −234 Hz and −46 Hz. Among these, two peaks (+0.7 ppm and -0.4 ppm) are relatively close to water and saturating them with spectral fat-sat methods would also saturate some of the water signal. In this work we saturate the fat-signal from the peaks at −420 Hz, −318 Hz, −472 Hz and −234 Hz. In order to achieve B1 uniformity high TWBP (>15) RF pulses were used for fat-sat. Variation in flip-angle (and the resultant T1 recovery effect) was used to vary the “darkness” of fat-sat with SHARP.
25 subjects were scanned using SPIR, SPAIR and SHARP fat-sat on a 3T MRI system (Magnetom Skyra, Siemens Healthineers, Erlangen, Germany) with typical turbo-spin-echo (TSE) sequence parameters for T2-weighted contrast using a trans/receive knee coil. Fat-sat uniformity was evaluated and compared between multiple SHARP options by two experienced radiologists.
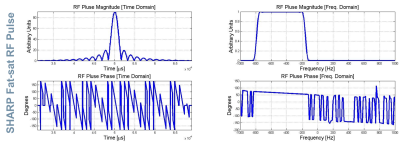
The impact of spectral characteristics (center frequency and full-width-at-half-maximum) of fat protons and variations in pulse type, offset, bandwidth and TBWP of SHARP on the uniformity of fat-sat were analyzed in 20 subjects to optimize SHARP fat-sat. Figure 1 shows the RF pulse characteristics for one of the optimized adaptive options used by SHARP. Five subjects were scanned with the optimized SHARP parameters (TBWP 26, bandwidth 630 Hz) and the features of SHARP were used to adapt the fat-sat frequency range (between which the saturation was performed) based on the subject specific spectrum for water and fat protons (fat-sat offset between -455 Hz to -485 Hz).
Results
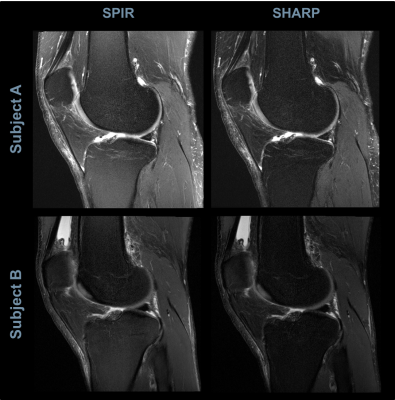
Figure 2 shows the comparison of fat-sat uniformity between SPIR and SHARP in a sagittal knee scan. SPIR had darker fat-sat near the joint and lighter fat-sat in the superior and inferior regions. SHARP demonstrates uniform level of fat-sat near the joint, superior and inferior regions.
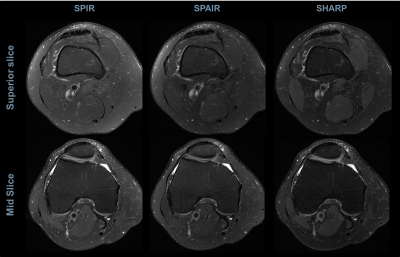
Figure 3 shows the comparison of uniformity between SPIR, SPAIR and SHARP fat-sat in an axial knee scan. Improvement in uniformity of the fat-sat and contrast between different tissue types can be observed with the SHARP fat-sat.
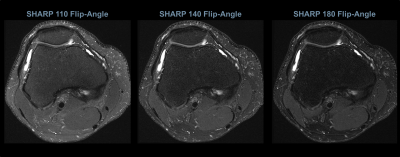
Figure 4 shows the comparison of SHARP fat-sat with different flip-angles. It can be observed that the “darkness” of the fat can be altered using appropriate flip-angle as per the clinical need.
Discussion
Achieving uniform fat-sat throughout the anatomy of interest is vital for clinical practice and the best method for fat-suppression depends on the anatomy and clinical need. Spectral fat-sat depends significantly on chemical separation of the water and fat-signal and hence a robust B0 is important. Even with second order shim, the B0 might be inhomogeneous in the case when metallic implants are present. In such scenarios SHARP might fail to achieve uniform fat-sat. However, for typical B0 inhomogeneities in the knee, SHARP achieved more homogeneous fat-sat compared to SPAIR which showed insufficient fat-sat in regions of significant B0 heterogeneity. Additionally, SHARP was shown to achieve better robustness to B1 variation compared to SPIR because of the use of high TBWP pulses.Conclusions
SHARP was shown to provide uniform suppression of the fat signal with robustness to B0 and B1 heterogeneity. Future work would focus on using SHARP in anatomical regions where spectral fat-sat methods are limited due to high B0 and B1 variability.Acknowledgements
We thank our colleagues Heiko Meyer, Wilfried Landschuetz, Andreas Schaefer and Dominik Paul for their helpful discussions and feedback.
References
1. Del Grande F, Santini F, Herzka DA, Aro MR, Dean CW, Gold GE, et al. Fat-Suppression Techniques for 3-T MR Imaging of the Musculoskeletal System. RadioGraphics. 2014 Jan;34(1):217–33.
2. Bley TA, Wieben O, François CJ, Brittain JH, Reeder SB. Fat and water magnetic resonance imaging. J Magn Reson Imaging. 2010 Jan 1;31(1):4–18.
3. Yu H, Shimakawa A, McKenzie CA, Brodsky EK, Brittain JH, Reeder SB. Multiecho water-fat separation and simultaneous R2* estimation with multifrequency fat spectrum modeling. Magn Reson Med. 2008;60:1122–1134.
Figures