5036
T2-mapping of Femoral Cartilage 3-months Following ACL Reconstruction Surgery1Mechanical Engineering, Stanford University, Stanford, CA, United States, 2Radiology, Stanford University, Stanford, CA, United States, 3Bioengineering, Stanford University, Stanford, CA, United States, 4Radiology, Massachusetts General Hospital, Boston, MA, United States, 5Electrical Engineering, Stanford University, Stanford, CA, United States, 6Mechanical Engineering, University of Saskatchewan, Saskatoon, SK, Canada
Synopsis
T2-mapping can be used to detect changes in cartilage following ACL injury that are indicative of cartilage degeneration. We imaged subjects at 3-weeks and 3-months post-ACL-reconstruction surgery to obtain T2 relaxation times for the femoral cartilage of both knees. A trend in increasing T2 relaxation times was observed for the injured knee at 3-months relative to 3-weeks, although this increase was not significant, while T2 remained consistent for the contralateral knee in this time. This work demonstrates that changes to cartilage may be occurring earlier than expected in the injured knee following ACL-reconstruction surgery.
Purpose
Patients who have experienced anterior cruciate ligament (ACL) tears have a significantly elevated risk of developing osteoarthritis, whether surgically reconstructed or not1,2. Quantitative MRI measures, such as T2, which is considered reflective of collagen content and organization3 have been used to track changes in cartilage following ACL injury4,5. At 1-year post-ACL-reconstruction, elevations in T2 times have been observed5. It is desirable to observe the earliest signs of cartilage degeneration in ACL injured patients to allow for the development and application of early interventional treatments to prevent further cartilage changes. The objective of this study was to determine if changes in T2 can be detected 3-months post-ACL-reconstruction surgery.Methods
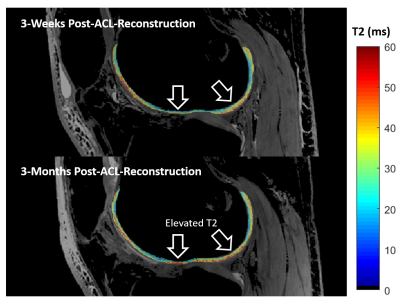
We scanned the ACL-reconstructed and contralateral knees of 5 subjects (4 females, ages 26-54) as part of a larger on-going study of 30 subjects over 2-years at a 3T MR scanner (GE Healthcare, Milwaukee, WI) using a 16-channel flexible knee coil. Subjects were excluded if they had a history of knee injury or surgery in the contralateral knee, a concomitant PCL tear in their ACL-injured knee, or a BMI > 35. Subjects were scanned 3-weeks and 3-months following surgery using a double-echo in steady-state sequence (DESS) in the sagittal plane with scan parameters: FOV=160mm, matrix=384x320, TE1/TE2/TR=6, 38, 22ms, slice thickness=1.5mm, flip angle=25°. T2 values were calculated from the two DESS echoes using a simple analytical model6 (Fig 1). The femoral cartilage was manually segmented from the sum-of-squares of the two DESS echoes (Seg3D, University of Utah). Segmented masks were then further automatically divided into the patellofemoral groove, medial condyle and lateral condyle. Differences between average T2 at 3-weeks and 3-months and differences between ACL-reconstructed and contralateral knees were compared using a general linear model (α<0.05).Results
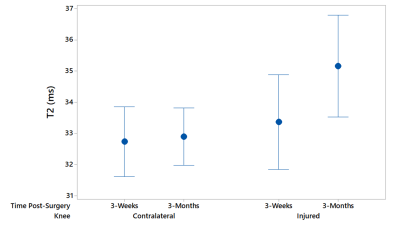
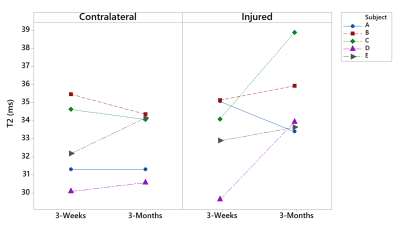
The average T2 in the femoral cartilage of ACL-reconstructed knees in all subjects increased from 3 weeks (average T2=33.4ms) to 3 months post-surgery (average T2=35.2ms) in the injured knee by 1.8ms, however it was not statistically significant. No significant change was observed in the contralateral knees in this same time, and the average T2 difference between 3 weeks (average T2=32.9) and 3 months (average T2=32.7ms) was only 0.2ms (Fig 2). The interaction between post-surgical time-point and knee (ACL-reconstructed or contralateral) did not reach significance in the general linear model (p=0.087). At 3 weeks post-op, there was little difference in T2 relaxation times between the injured and contralateral knee, but at 3 months post-op the T2 values of the injured knee were higher than in the contralateral knee by 2.4ms, which also was not significant (Fig 2). Looking individually at subjects, ACL-reconstructed knees showed an increase in T2 times from 3 weeks to 3 months in 4 out of 5 subjects (Fig 3).Discussion
We observed a trend of increasing T2 relaxation times from 3-weeks to 3-months post-surgery for ACL-reconstructed knees, whereas T2 relaxation times in contralateral knees were consistent between these time points. We have previously shown that our DESS T2 measurements are repeatable within a 3% coefficient of variation6. T2 elevations 3-months post-surgery are consistent with the small increases previously seen in T2 times 1-year post-ACL-reconstruction5, suggesting that the changes in cartilage leading to elevated T2 may be occurring much earlier following ACL-reconstruction surgery than expected. The difference in T2 between healthy and osteoarthritic femoral cartilage in one year has been shown to be approximately 5ms8.9, which is just over 2x the difference in T2 times we saw in our study in under 3-months. Changes to T2 between 3 weeks and 3 months post-surgery could also be an effect of a subject’s modified mobility and reduced weight-bearing of the injured knee at these times, or a result of post-surgical inflammation. Patients are still relying on crutches 3-weeks post-surgery and are then walking 3-months post-surgery. These early changes in T2 may be indicative of degenerative changes occurring in the cartilage of the ACL-reconstructed subjects, but a larger sample size of ACL-reconstructed subjects and long-term follow-up of these subjects will be necessary to understand if these early changes are correlated with osteoarthritis. Being able to identify when the earliest degenerative cartilage changes occur can allow for the development and application of interventional osteoarthritis treatments aimed at preventing further cartilage degeneration.Conclusion
Femoral cartilage T2 relaxation times increasing from 3-weeks to 3-months post-surgery for ACL injured subjects suggest that degenerative cartilage changes may be happening within 3-months of ACL reconstruction surgery. Additional subjects are in the process of being recruited and will help further elucidate trends in cartilage T2 relaxation times following ACL-reconstruction surgery.Acknowledgements
NIH R01 AR0063643, NIH R01 EB002524, NIH K24 AR062068, and GE Healthcare.References
[1] David Simon, Randy Mascarenhas, Bryan M. Saltzman, Meaghan Rollins, Bernard R. Bach Jr., and Peter MacDonald, “The Relationship between Anterior Cruciate Ligament Injury and Osteoarthritis of the Knee,” Advances in Orthopedics, vol. 2015, Article ID 928301, 11 pages, 2015. doi:10.1155/2015/928301
[2] Meuffels DE, Favejee MM, Vissers MM, et al. “Ten year follow-up study comparing conservative versus operative treatment of anterior cruciate ligament ruptures. A matched-pair analysis of high level athletes.” British Journal of Sports Medicine 2009;43:347-351.
[3] Nieminen, Miika & Rieppo, Jarno & Töyräs, Juha & Hakumäki, Juhana & Närväinen, Johanna & M. Hyttinen, Mika & Helminen, Heikki & Jurvelin, Jukka. (2001). T2 relaxation reveals spatial collagen architecture in articular cartilage: A comparative quantitative MRI and polarized light microscopic study. Magnetic Resonance in Medicine. 46. 487 - 493. 10.1002/mrm.1218.
[4] Li, X., Kuo, D., Theologis, A., Carballido-Gamio, J., Stehling, C., Link, T. M., … Majumdar, S. (2011). Cartilage in Anterior Cruciate Ligament–Reconstructed Knees: MR Imaging T1ρ and T2—Initial Experience with 1-year Follow-up. Radiology, 258(2), 505–514. http://doi.org/10.1148/radiol.10101006
[5] Su, F., Hilton, J. F., Nardo, L., Wu, S., Liang, F., Link, T. M., … Li, X. (2013). Cartilage Morphology and T1ρ and T2 Quantification in ACL-reconstructed Knees: A 2-year Follow-up. Osteoarthritis and Cartilage / OARS, Osteoarthritis Research Society, 21(8), 1058–1067. http://doi.org/10.1016/j.joca.2013.05.010
[6] B. Sveinsson, A.S. Chaudhari, G.E. Gold, B.A. Hargreaves, A simple analytic method for estimating T2 in the knee from DESS, In Magnetic Resonance Imaging, Volume 38, 2017, Pages 63-70, ISSN 0730-725X, https://doi.org/10.1016/j.mri.2016.12.018.
[7] Chaudhari, A.S., Black, M.S., Eijgenraam, S., Wirth, W., Maschek, S., Sveinsson, B., Eckstein, F., Oei, E.H.G., Gold, G.E. and Hargreaves, B.A., 2017. Five-minute knee MRI for simultaneous morphometry and T2 relaxometry of cartilage and meniscus and for semiquantitative radiological assessment using double-echo in steady-state at 3T. Journal of magnetic resonance imaging: JMRI.
[8] Li X Benjamin Ma C Link TM Castillo DD Blumenkrantz G Lozano J Carballido-Gamio J Ries M Majumdar S. In vivo T(1rho) and T(2) mapping of articular cartilage in osteoarthritis of the knee using 3 T MRI. Osteoarthritis Cartilage. 2007;15:789–97.
[9] Dunn TC, Lu Y, Jin H, Ries MD, Majumdar S. T2 relaxation time of cartilage at MR imaging: comparison with severity of knee osteoarthritis. Radiology 2004;232:592–598.
Figures