5027
Performance of ultrafast DCE-MRI for diagnosis of prostate cancer1Department of Radiology, University of Chicago, Chicago, IL, United States, 2Sino-Dutch Biomedical and Information Engineering School, Northeastern University, Shenyang, China, 3Research Computing Center, University of Chicago, Chicago, IL, United States, 4Department of Pathology, University of Chicago, Chicago, IL, United States
Synopsis
This study aimed to test high temporal resolution DCE- MRI for different zones of the prostate and evaluate its performance in the diagnosis of prostate cancer (PCa). High temporal resolution (~2.2s) was achieved by modestly decreasing spatial resolution, increasing sensitivity encoding and partial Fourier factors. Our results show that PCa had significantly faster signal enhancement and washout rates than normal tissue. DCE-MRI with higher temporal resolution may capture clinically useful information for PCa diagnosis that would be missed by low temporal resolution DCE-MRI. This new information could improve the performance of mpMRI in prostate cancer detection.
Introduction
The full potential of dynamic contrast enhanced (DCE) MRI may not be reached and particularly, the details of the contrast uptake kinetics may not be captured with low temporal resolution. Higher temporal resolution has been shown to increase diagnostic performance in prostate cancer (PCa) detection (1). The aim of the study is to test high temporal resolution DCE- MRI for different zones of the prostate and evaluate its performance in the diagnosis of prostate cancer (PCa). Determine whether the addition of ultrafast DCE-MRI improves the performance of mpMRI. An Empirical Mathematical Model (EMM) (2) is used to characterize patterns of signal enhancement with a temporal resolution of DCE-MRI close to 2 seconds, which is significantly faster than clinical routine DCE-MRI of the prostate.Methods
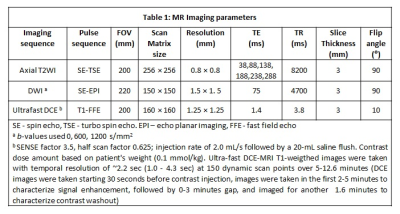
Patients (n=20) with pathologically confirmed PCa underwent preoperative MRI on 3T Philips Achieva scanner with T2-weighted, diffusion-weighted and high temporal resolution (~2.2sec) DCE-MRI using gadoterate meglumine (Guerbet LLC) without an endorectal coil. High temporal resolution was achieved by modestly decreasing spatial resolution, increasing sensitivity encoding and partial Fourier factors (SENSE factor 3.5, half scan factor 0.625) and decreasing the field-of-view to allow a small amount of aliasing (see Table 1). DCE-MRI data was analyzed by fitting signal intensity with an EMM to obtain parameters: percent signal enhancement, enhancement rate (α), washout rate (β), initial enhancement slope and enhancement start time along with ADC and T2 values.
The baseline signal intensity value (S0) of each voxel was calculated by averaging the signal intensity (S(t)) of the five pre-contrast time points. The percent signal enhancement (PSE) was calculated using the following equation:
$$PSE (t)= \frac{S(t)-S_{0}}{S_{0}}\times100$$
The PSE curve was fitted with the EMM on a voxel-by-voxel basis using a nonlinear least-squares algorithm using the following equation:
$$PSE(t)=A (1-e^{-\alpha t}) e^{-\beta t}$$
where A is the amplitude of PSE, α is the signal enhancement or uptake rate (sec-1) and β is the washout rate (sec-1). The maximum intensity projections (MIPs) were generated by finding the maximum PSE value of each voxel. The initial time of enhancement (start point) for each voxel was determined by an iterative process. The initial signal enhancement slope was measured as the slope of the PSE over the time period beginning at the time of initial enhancement and continuing for ten time points. The time of arrival (TOA) of contrast media in each voxel was defined as the time at which PSE achieved 20% signal enhancement. Regions of interests were placed on sites of prostatectomy verified malignancy (n=46) and normal tissue (n=71) from different zones to calculate the above mentioned metrics for subsequent statistical analysis.
Results
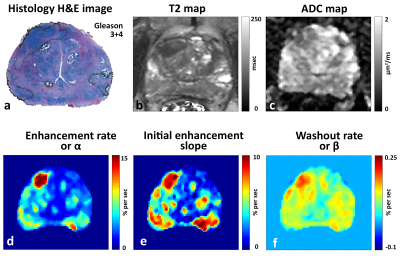
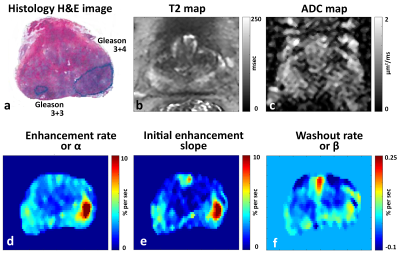
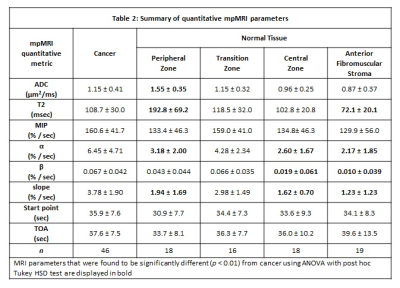
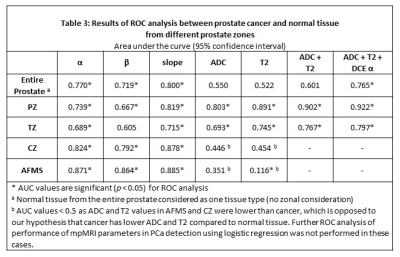
Representative images showing reduced ADC and T2 values and increased α, β and slope in ROIs denoting cancerous lesions and corresponding histology images are shown in Figures 1 and 2. Cancer (α=6.45±4.71s-1, β=0.067±0.042s-1, slope=3.78±1.90s-1) showed significantly (p<0.05) faster signal enhancement and washout rates than normal tissue (α=3.0±2.1s-1, β=0.034±0.050s-1, slope=1.9±1.4s-1), but showed similar percentage signal enhancement and enhancement start time. Table 2 provides detailed results from different prostatic zones. ROC analysis showed area under the curve (AUC) for DCE parameters were comparable to ADC and T2 in the peripheral (DCE 0.67-0.82, ADC 0.80, T2 0.89) and transition zones (DCE 0.61-0.72, ADC 0.69, T2 0.75) but higher in central zone (DCE 0.79-0.88, ADC 0.45, T2 0.45) and anterior fibromuscular stroma (DCE 0.86-0.89, ADC 0.35, T2 0.12) (see Table 3). Importantly, combining DCE with ADC and T2 increased AUC by ~30%, further improving the diagnostic accuracy of PCa detection.Discussion
Our results show that high temporal resolution or ultrafast DCE-MRI is feasible and could improve the diagnosis of prostate cancer. PCa had significantly faster signal enhancement and washout rates than normal tissue. While the contrast media arrival time to the benign prostate and PCa was similar, the faster rate of initial enhancement characterized by α, leads to the wrong impression of early enhancement. Ultrafast DCE-MRI increases sensitivity to initial rate of enhancement, and initial time of enhancement. ROC analysis showed that AUCs for DCE-MRI parameters were comparable to those for ADC and T2 in the peripheral and transition zones but higher in central zone and anterior fibromuscular stroma. Importantly, combining DCE parameters with ADC and T2 further improved the diagnostic accuracy of PCa detection.Conclusion
Quantitative parameters from EMM fits to ultrafast DCE-MRI improve diagnosis of PCa. DCE-MRI with higher temporal resolution may capture clinically useful information for PCa diagnosis that would be missed by low temporal resolution DCE-MRI. This new information could improve the performance of mpMRI in prostate cancer detection.Acknowledgements
The study was funded by Guerbet LLC, Philips Healthcare and National Institutes of Health (NIH R01 CA172801 and NIH 1S10OD018448-01).References
1. Othman AE, Falkner F, Weiss J, Kruck S, Grimm R, Martirosian P, Nikolaou K, Notohamiprodjo M. Effect of Temporal Resolution on Diagnostic Performance of Dynamic Contrast-Enhanced Magnetic Resonance Imaging of the Prostate. Invest Radiol 2016;51(5):290-296.
2. Fan X, Medved M, River JN, Zamora M, Corot C, Robert P, Bourrinet P, Lipton M, Culp RM, Karczmar GS. New model for analysis of dynamic contrast-enhanced MRI data distinguishes metastatic from nonmetastatic transplanted rodent prostate tumors. Magnetic Resonance in Medicine 2004;51(3):487-494.
Figures