5003
Quantitative Susceptibility Mapping of Articular Cartilage in Patients with OsteoarthritisHongjiang Wei1, Huimin Lin2, Yuyao Zhang1, Weibo Chen3, Fuhua Yan2, and Chunlei Liu1
1University of California, Berkeley, Berkeley, CA, United States, 2Department of Radiology, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China, 3Philips Healthcare, Shanghai, Shanghai, China
Synopsis
Osteoarthritis (OA) is a multifactorial degenerative joint disease and is the most common form of arthritis which characterized by degenerative changes in the cartilage, menisci,
Introduction
Osteoarthritis (OA) is a multifactorial degenerative joint disease and is the most common form of arthritis. Characterized by degenerative changes in the cartilage, menisci, ligaments and bone, OA is considered a disease of the whole joint. Recent work has shown varying magnetic susceptibility in different anatomical structure of the knee at 7 T. Bone and marrow have very short T2* at 7 T; therefore, the bone areas are masked out to prevent inaccurate magnetic susceptibility estimation caused by the ill-posed inverse problem. In this study, we have implemented an improved compressed sensing (iCS) method for QSM reconstruction that can provide the susceptibility maps of the whole knee joints. A significantly lower level of streaking artifacts is observed in the resulting susceptibility maps of knee joints including bone regions. Our results showed that bone marrow lesions in OA exhibit more paramagnetic susceptibility than surroundings and a clearer change in susceptibility distribution was observed in patients with cartilage damage.Methods
MRI was performed on the knees of volunteers and patients with OA with approval of the institutional review board and informed consent from the subjects. All images were acquired with a Philips Ingenia 3T MRI scanner. An axial 3D gradient echo sequence was used to acquire images with the following parameters: TE1/spacing/TE6=2.5/1.0/6.7ms, TR=40ms, flip angle=15°, matrix size=160×160×160, voxel size=1×1×1mm3. A sagittal 3D gradient echo sequence with fat saturation was used to image the cartilage with higher spatial resolution: TE =5.2 ms, TR=20 ms, flip angle=15°, matrix size=560×560×90, voxel size=0.28×0.28×2mm3. Compressed sensing (CS) is used to compensate for k-space regions where direct filter inversion is unstable1. In this study, by using a non-linear formation of the measured phase to magnetic susceptibility2 and incorporating the k-space under-sampling and weighting, the proposed improved method (iCS) essentially solves this equation: $$$χ=min{|| F-1·Wkspace·F(exp(F-1D2·Fχ)-exp(φ))||2+ λ1·||ψχ||1 +λ2·TV(χ)} $$$(1). F and F-1are Fourier transform and inverse Fourier transform, respectively.ψ is wavelet transform. TV stands for total variation. λ1 and λ2 are the penalty terms. Wkspace is the k-space weighting term and we adopted D2 for k-space weighting, which extended the concept of compressed sensing in the sense that the D2 term has a conical surface with the coefficient is close to zero. Eq. 1 can be solved iteratively using the conjugate gradient (CG) solver. In this study, the chemical shift effect is removed using a water-fat separation method3 for multi-echo data and field map was estimated, wrapped phase was unwrapped using Laplacian-based phase unwrapping method and the background phase was then removed using the V_SHARP method3.Results
As illustrated in Fig. 1, after removing the chemical shift effect, the multilayer structure of the cartilage is clearly observed in the data (1mm resolution) produced by iCS with λ1=1xe-4 and λ2=2xe-5. Moreover, the computed magnetic susceptibility provides clear contrast between the bone marrow lesion and surroundings in a representative knee patient. With higher spatial resolution, the layer structure revealed by QSM in a healthy subject is shown in Fig. 2a. The susceptibility appears more diamagnetic (colored by blue) in the deep zone and relatively more paramagnetic in the superficial zone which is consistent with previous studies on cartilage using QSM at 7 T3. Fig. 2b shows representative MRI images of articular cartilage in a patient with cartilage damage. The thinned cartilage in patellar with severe thickness loss is observed from magnitude and proton density weighted (PDW) images. Interestingly, QSM provides a more detailed abnormality, e.g. the multilayer ultrastructure is missing compared with that of the healthy volunteer.Discussion
We have implemented a new QSM reconstruction algorithm that allows the quantification of magnetic susceptibility of whole knee tissues. With the proposed QSM reconstruction method, the multiple layer pattern of the cartilage can be revealed even at 1 mm isotropic spatial resolution acquired at 3T. It allows depiction and quantification of the magnetic susceptibility of bone marrow regions. Moreover, clear susceptibility contrast change was observed in patients with cartilage loss. Specifically, at higher spatial resolution, the multilayer ultrastructure revealed by different magnetic susceptibility is missing compared with that of healthy subjects, indicating the microstructure alterations or changes in the constituents of the cartilage. E.g., changes in water and proteoglycan contents of articular cartilage and causes breakdown of the collagen molecules, altering the structural integrity and organization of the collagen fiber network.Conclusion
QSM allows in vivo imaging and quantification of the magnetic susceptibility of the knee in patients with osteoarthritis at 3 T. QSM may have the potential to provide a new way to characterize knee tissue microstructural changes related to the disease.Acknowledgements
This work was supported, in part, by the ISMRM Research Exchange Program.References
1. Wu, B., et al., Whole brain susceptibility mapping using compressed sensing. Magnetic resonance in medicine, 2012. 67(1): p. 137-147. 2. Liu, T., et al., Nonlinear formulation of the magnetic field to source relationship for robust quantitative susceptibility mapping. Magnetic resonance in medicine, 2013. 69(2): p. 467-476. 3. Wei, H., et al., Investigating magnetic susceptibility of human knee joint at 7 tesla. Magnetic resonance in medicine, 2017.Figures
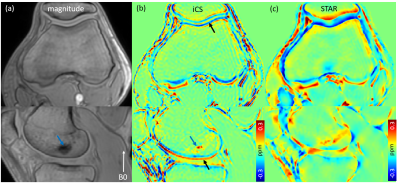
Fig.1. Representative MRI images show knee joints in a patient with a bone marrow lesion. (a) Magnitude image, (b) susceptibility maps reconstructed using the proposed method (iCS) and (c) using the STAR method. Blue arrows point to the bone marrow lesion and black arrows indicate the multilayer structure of the articular cartilage.
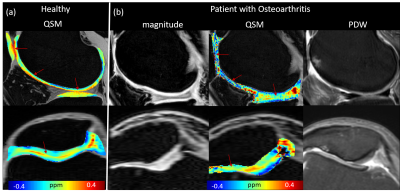
Fig.2. Representative MRI images show articular cartilage in a healthy subject and a patient with cartilage damage. Magnitude and proton density weighted images clearly show cartilage thinning. Color map of susceptibility show clear cartilage ultra-layer pattern from deep zone to superficial zone in a healthy subject. This multilayer ultrastructure in the cartilage disappears in patient with thinned cartilage as indicated by red arrows in (b).