4951
Transient neuronal dysfunction correlates with hypo-perfusion in patients with moderate post-traumatic brain injury1Department of Radiology / Neuroradiology Division, Massachusetts General Hospital/ A.A. Martinos Center for Biomedical Imaging, Charlestown, MA, United States, 2Harvard Medical School, Boston, MA, United States, 3Department of Radiology, Massachusetts General Hospital/ A.A. Martinos Center for Biomedical Imaging, Charlestown, MA, United States, 4Department of Radiology, Massachusetts General Hospital, Boston, MA, United States, 5Wellman Center for Photomedicine, Department of Dermatology, Massachusetts General Hospital, Boston, MA, United States, 6Department of Emergency Medicine, Massachusetts General Hospital, Boston, MA, United States, 7Department of Physical Medicine & Rehabilitation, Spaulding Rehabilitation, Charlestown, MA, United States, 8Department of Emergency Medicine and Department of Surgery, Massachusetts General Hospital, Boston, MA, United States, 9Emergency Radiology and Emergency Neuroradiology, Massachusetts General Hospital, Boston, MA, United States
Synopsis
We present a DOD funded study to assess the effects of low-level light therapy (LLLT) on metabolites measured by MRS and cerebral perfusion measured by ASL using a double-blind, placebo controlled study where patients with moderate TBI were randomized between LLLT and sham treatment. We report CBF and metabolic changes pertaining to neuronal injury and neuroinflammation for the entire cohort (i.e., both treated and control arms), before the blind is broken. Our findings suggest that transient neuronal dysfunction in the posterior cingulate cortex and neuroinflammation in the thalamus correlated with hypo-perfusion during the subacute phase of moderate TBI.
INTRODUCTION
Not many treatment options are currently available to treat traumatic brain injury (TBI). Low-level light therapy (LLLT) has been reported to improve recovery in TBI and stroke models [1-3]. This study is designed to assess the effects of LLLT on metabolites measured by MR spectroscopy and cerebral perfusion measured by arterial spin labeling (ASL) using a double-blind, placebo controlled study where patients with moderate TBI were randomized between LLLT and sham treatment. MRS has been utilized in the assessment of TBI due to its ability to measure brain metabolite concentrations. The pertinent metabolites detected are sensitive to neuronal injury, neuroinflammation, hypoxia, energy dysfunction, and membrane turnover, all conditions implicated in TBI [4]. There is increasing evidence that neurovascular dysregulation contributes to persistent symptoms in patients with TBI. ASL is able to measure cerebral blood flow (CBF) non-invasively. Here we report perfusion changes and metabolic changes pertaining to neuronal injury and neuroinflammation for the entire cohort (i.e., both treated and control arms), before the blind is broken.METHODS
Participants: Twenty-six patients with moderate TBI (age: 20-79 years, 14F/12M), and Glasgow Coma Scale (GCS) score between 9 and 11, or GCS between 12 and 15 with abnormal imaging findings, were enrolled. Signed informed consent was obtained from participants prior to all experimental procedures. Clinical assessments including the Rivermead Post-Concussion Symptoms Questionnaire (RPQ) were performed at baseline, 2 weeks, 3 months, and 6 months after injury.
Therapy: Each patient in the study arm received light therapy three times using a Photomedex helmet emitting Near-Infrared light. The light therapy sessions were administered daily for 3 days, each lasting 20 minutes, and separated by at least 12 hours, with the first one commencing within 72 hours of injury. For the patients in the sham arm, all procedures were the same except the NIR light was not turned on.
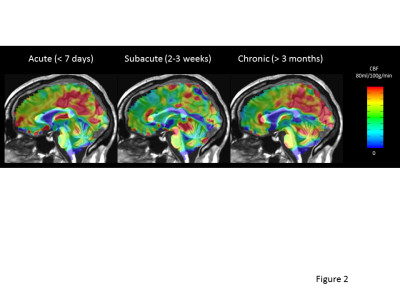
MR Methods: MRI scanning was performed at acute/baseline (within 7 days after injury), subacute (2-3 weeks) and chronic (more than 3 months) stages after injury on a 3-Tesla scanner (Prisma™, Siemens, Germany). Imaging included 1) 3D-MEMPRAGE; 2) pulsed arterial spin labeling (PASL) and 3) 2D MRSI (TE 40ms and 135ms, TR 1700ms.) (See Figure 1 for representative VOI placement).
MRSI data analysis: LCModel was used to analyze the MRS data and to measure brain metabolites pertaining to neuronal viability (N-Acetylaspartate/Creatine, NAA/Cr) and neuroinflammation (myo-inositol, mI/Cr). For data analysis, we focused on the left and right posterior cingulate cortex (PCC) and left and right thalami.
Statistical Analysis: To explore the temporal metabolic changes, paired t-tests were used between time points. To explore correlations between metabolites and CBF and clinical performance, Pearson correlation coefficients were calculated.
RESULTS
Figure 2 shows a representative longitudinal perfusion pattern that was observed in over 80% of patients; CBF transiently decreases at the 2-week follow-up scan compared to the baseline scan and then rebounds at 3 months; this pattern was most apparent in the thalami, PCC, precuneus and insula. Based on these findings, we chose to explore metabolic changes in the left and right PCC and thalami.
NAA/Cr, the marker for neuronal integrity, showed transient decreases at 2 weeks (during the subacute phase of TBI) in the left and right PCC, followed by a rebound 3 months later (Figure 3A). NAA/Cr did not significantly change in the thalami (Figure 3B). We found positive correlations between the NAA/Cr in the left and right PCC and global CBF at timepoints 1 and 3 (Table 1). While mI/Cr was not significantly different over time in the combined cohorts, we found that global CBF was negatively correlated with mI/Cr in the thalami; an increase in mI/Cr correlated with decreased perfusion (Table 1).
Lastly, we correlated NAA/Cr and
mI/Cr levels at baseline with post-concussion symptoms at baseline and 6 months. MI/Cr in the left and right thalamus correlated with the
summation of scores from 13 psychological and social function related symptoms (RPQ-13)
at baseline, and NAA/Cr in the left and right PCC correlated with RPQ-13 at 6
months (Table 2).
CONCLUSION
Our findings suggest that transient neuronal dysfunction in the PCC and neuroinflammation in the thalamus correlated with hypo-perfusion during the subacute phase of TBI. Furthermore, NAA/Cr levels in the PCC correlated with long-term post-concussion symptoms, while mI/Cr in the thalamus reflected the baseline post-concussion symptoms. Limitations of this study include small sample size. Since patient enrollment is continuing, and the blind in the LLLT study has not been broken, how light therapy modulates the metabolism is unknown at this time.Acknowledgements
This study was supported by DoD grant W81XWH-13-2-0067.References
1. Ando, T., et al., Comparison of therapeutic effects between pulsed and continuous wave 810-nm wavelength laser irradiation for traumatic brain injury in mice. PLoS One, 2011. 6(10): p. e26212.2. Sharma, S.K., et al., Dose response effects of 810 nm laser light on mouse primary cortical neurons. Lasers Surg Med, 2011. 43(8): p. 851-9.
3. Wu, Q., et al., Low-level laser therapy for closed-head traumatic brain injury in mice: effect of different wavelengths. Lasers Surg Med, 2012. 44(3): p. 218-26.
4. Marino, S., et al., 1H-MR spectroscopy in traumatic brain injury. Neurocrit Care, 2011. 14(1): p. 127-33.
Figures
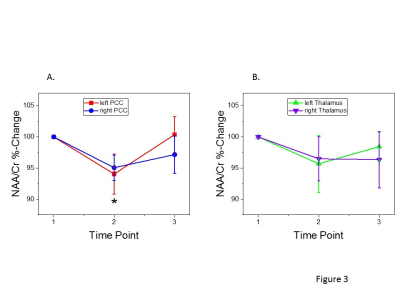
A) NAA/Cr showed transient decreases at 2 weeks in the left PCC (p = 0.03) and right PCC (p = 0.01) , followed by a rebound 3 months later.
B) NAA/Cr did not significantly change in the thalami.
Error bars indicate standard error of the mean
Pearson Correlations between metabolites and cerebral blood flow.
Dashes indicate non-significant correlations
Pearson Correlations between metabolites and clinical assessment.
Dashes indicate non-significant correlations.