4950
Military TBI Patients Demonstrate Increased Cerebral Venous Volume Using Quantitative Susceptibility Mapping1National Intrepid Center of Excellence, Walter Reed National Military Medical Center, Bethesda, MD, United States, 2The NorthTide Group, LLC, Sterling, VA, United States
Synopsis
Cerebral venous volume above the lateral ventricle was analyzed using quantitative susceptibility mapping in patients with severe (n = 7), moderate (n = 21) and mild (n = 27 for blast and n = 19 for nonblast) TBI. Severe and moderate TBI patients both demonstrated increased venous volume compared to control subjects without history of TBI. Blast injured mild TBI patients also showed increased venous volume compared to the control subjects. These results suggest that microvascular injury may present in TBI patients and blast related injury might have a more pronounced impact on the venous system.
Introduction
Microvascular injury is a near universal finding in animal models of TBI1. In patients who died of severe TBI, microscopic perivascular petechial hemorrhages were observed even when macroscopic hemorrhage was absent on gross examination of the brain. In particular, small capillaries and vessels exhibited more perivascular microhemorrhages than larger vessels2. In these patients, abundant intravascular microthrombi in the arterioles and venules primarily affected microvessels of 6 to 100 um diameter3. Due to the highly invasive nature of this type of analysis, there are limited reports on the venous characteristics in TBI patients who survived the injury. Quantitative susceptibility mapping (QSM) provides the opportunity to analyze venous structure noninvasively. This investigation aims to characterize venous involvement of small vessels in TBI patients using QSM4.Methods
This retrospective study included 7 patients with severe TBI (severe, 36 ± 5 years old), 21 patients with moderate TBI (moderate, 35 ± 8 years old), 27 mild TBI patients with blast injury (mild-blast, 30 ± 7 years old), 19 mild TBI patients with non-blast injury (mild-nonblast, 30 ± 11 years old) and 19 control subjects without history of TBI (control, 32 ± 6 years old). The inclusion criteria are male, images with good QA, and mild TBI with time since injury less than 6 months. Control participants with hypertension were excluded.
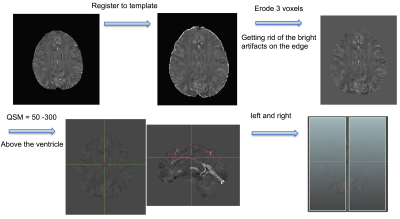
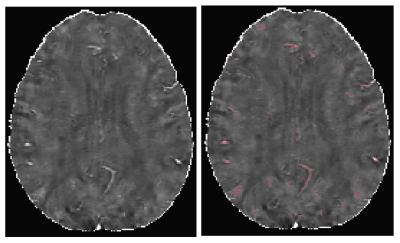
Images were acquired on a 3T scanner with a 32-channel phased array head coil. The images used for QSM were acquired using a 3D flow-compensated multi-echo gradient-echo sequence with TR = 45 ms, 5 echoes, TE0 = 13 ms, echo-spacing = 6 ms, FA = 20°, FOV = 24 × 24 cm2, 512 × 256 matrix, 88 slices at 1.5 mm thickness. QSM images were calculated using a software package provided by our collaborator4. Figure 1 illustrates the processing pipeline. To minimize the contribution from large vessels, the relatively homogeneous brain area above the lateral ventricle was chosen as the ROI. A threshold between 50 – 300 ppm was applied to this brain area (whole) on QSM images. A thin gap of 6 voxels at the midline was excluded in the right and left ROIs to minimize the susceptibility effects of the large vessels around midline.
Results
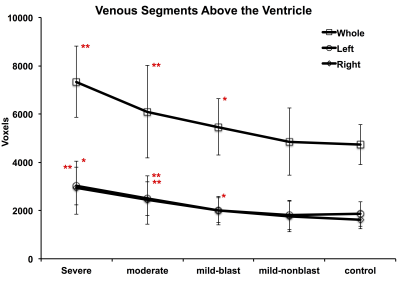
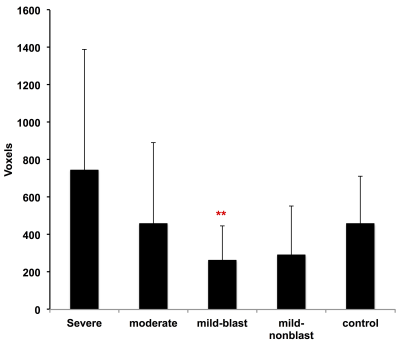
Severe and moderate TBI patients both demonstrated increased venous volume compared to controls: 7339 ± 1475 voxels (p < 0.01) for severe TBI and 6093 ± 1917 voxels (p < 0.01) for moderate TBI vs. 4272 ± 830 voxels for controls in the whole ROI; 3018 ± 784 voxels (p < 0.01) for severe TBI and 2491 ± 700 voxels (p< 0.01) for moderate TBI vs. 1855 ± 507 voxels for controls in the left; 2950 ± 1103 voxels (p< 0.05) for severe TBI and 2439 ± 1007 voxels (p < 0.01) for moderate TBI vs. 1614 ± 369 voxels for controls in the right. Blast injured mild TBI patients also demonstrated increased volume compared to controls: 5643 ± 1163 voxels (p < 0.05) in the whole ROI and 1992 ± 586 voxels (p< 0.05) in the right. Mild TBI patients due to nonblast injury were not different from the controls: 4853 ± 830 voxels in the whole ROI, 1855 ± 602 voxels in the left and 1749 ± 634 voxels in the right. In addition, mild TBI patients showed more evenly distributed venous volumes (less difference between the right and left ROIs) compared to control subjects: 262 ± 185 voxels (p< 0.01) for blast and 292 ± 258 voxels (p = 0.07) for nonblast vs. 457 ± 255 voxels for controls.Discussion and Conclusion
Patients with severe and moderate TBI both demonstrated increased venous volume above the lateral ventricle compared to controls. Mild TBI patients with blast injury also exhibited an increase in venous volume but those with nonblast injury were not different from the controls. Blast injured mild TBI patients also demonstrated more evenly distributed venous volumes in the right and left ROIs. These results suggest that microvascular injury may present in military TBI patients. The results also suggest that blast related TBI has a more pronounced impact on the venous system compared to nonblast TBI. Microhemorrhage, which adds to the total segmented volume using this threshold approach, could be a confounding factor. However, removing patients with micorhemorrhage demonstrated similar results (data not shown) indicating the results are not driven by the presence of micorhemorrhage.Disclaimer:
The views expressed in this abstract are those of the authors and do not reflect the official policy of the Department of Army/Navy/Air Force, Department of Defense, or U.S. Government.Acknowledgements
We would like to acknowledge our grant support: #13129004 "Advanced imaging acquisition and data analysis for a military TBI Neuroimaging database" from USAMRMC.References
1. Kenny K et al. Experimental Neurology 2016;275:353-366.
2. Oppenheimer DJ, J. Enurol Enurosurg Psychiatry 1968, 31:299-306.
3. Stein SC et al. Enrosurgery 2004; 54:687-691.
4. Liu T et al. Magn Reson Med 2011; 66:777-783.
Figures