4912
Effects of sex and age on CMR-derived left ventricular wall thickness and peak systolic wall stress in normal subjectsXiaodan Zhao1, Angela S Koh1,2, Soo Kng Teo3, Sen Lin2, Shuang Leng1, Ris Low1, Yi Su3, Ru San Tan1,2, and Liang Zhong1
1National Heart Centre Singapore, Singapore, Singapore, 2Duke-NUS Medical School Singapore, Singapore, Singapore, 3Institute of High Performance Computing, A*STAR, Singapore, Singapore, Singapore
Synopsis
To investigate the left ventricular (LV) wall thickness, LV wall stress and their association with age and sex in a cohort of 210 healthy subjects (age: 19 to 87 years), endocardial and epicardial contour meshes from stacks of 2D short axis images were imported into our in-house software (CardioWerkz) for further analysis of 3D regional wall thickness and peak systolic wall stress (PSWS). Results indicated that mean LV wall thickness was smaller in females than males, and more positively correlated with age in female than male. Moreover, no significant difference for mean PSWS between females and males.
Background and Purpose
Left ventricular (LV) wall thickness increases with age. Inversely related to wall thickness, LV wall stress is a physiological index of cardiac compensation due to LV remodeling with ageing and disease. The interaction between age and sex on LV wall thickness and stress has not been well studied. We aimed to study the effects of sex and age on LV wall thickness and stress in normal subjects.Methods
Single-centre study with prospective enrollment of volunteers without known cardiovascular disease, who all underwent cardiovascular magnetic resonance (CMR) imaging on a 3.0T scanner (Philips, Ingenia). LV end-diastolic (ED), end-systolic (ES) volumes and mass were calculated using Simpson’s method from semi-automatically derived endocardial and epicardial contours in stacks of LV short-axis cine CMR slices, with co-registered valve planes defined on LV long-axis views. Reconstructed temporally-resolved 3D endocardial and epicardial mesh coordinates were input into an in-house software (CardioWerkz) for analysis of LV regional wall thickness and peak systolic wall stress (PSWS) based on standard American Heart Association 17-segment heart model but omitting the apex, where thickness is assumed to approximate zero. PSWS was evaluated as 0.133*0.9*SBP*[(R/T)/(2+(1+T/2R)], where SBP is arm-cuff systolic blood pressure; and R and T respectively the regional LV radius and wall thickness calculated from 3D LV endocardial and epicardial geometries, where one-to-one correspondence of mesh vertices at all temporal phases were realized based on point-surface curvedness and conservation of energy. Global mean values of these parameters were compared, stratified by sex. Linear correlation analyses between age and the mean of these regional parameters were performed for the entire cohort, as well as within the male and female groups.Results
We enrolled 210 subjects (age range 19 to 87 years; male-female ratio 111:99). Compared with males, females had significantly smaller body surface area and indexed LV volumes and mass (all P < 0.05), similar LV ejection fraction (P = NS), smaller wall thicknesses at both ED and ES phases, similar mean PSWS (P = 0.950) (Table 1), and similar regional PSWS at basal, mid and apical LV levels (Figure 1). Wall thickness correlated with age for the whole cohort, but only in females and not in males when analysis was stratified by sex (Table 2). No significant correlation was found between PSWS and age in the whole cohort, and within both male (r = -0.117, P = NS) and female groups (r = -0.065, P = NS).Conclusion
In females without prior cardiovascular disease, mean LV wall thickness was smaller compared to males; and appeared to positively correlate with age, more so than in males. No significant difference was observed for mean PSWS between males and females, and no association was seen between mean PSWS and age, implying that noninvasive CMR-derived mean PSWS may be a suitable candidate index for early detection and longitudinal monitoring of sex- and age-independent myocardial decompensation in ageing and disease.Acknowledgements
No acknowledgement found.References
No reference found.Figures
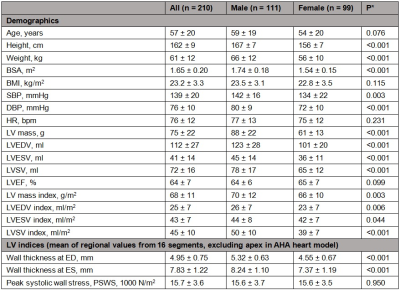
Table 1.
Comparison of subjects’ demographics and left ventricular regional indices,
stratified by sex.
AHA = American Heart Association, ED =
end-diastole; ES = end-systole, LV = left ventricle. *Comparison between the male and female groups
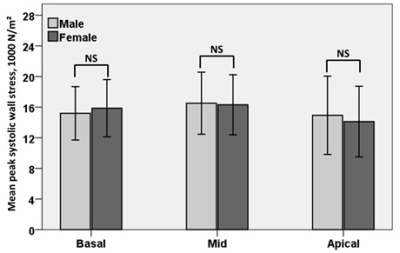
Figure 1. Comparison of regional peak systolic wall
stresses at basal, mid and apical levels between males and females.
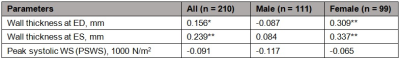
Table 2. Pearson correlation coefficients between age
and mean of left ventricular regional indices in the entire cohort, male and
female subjects. *P <
0.05; **P < 0.01