4878
Free-Breathing Myocardial T1-Acquisition with Region-based Analysis is Feasible to Quantify Diffuse Myocardial Fibrosis1Dpt of Medical Imaging, National Taiwan University Hospital, Taipei, Taiwan, 2Dpt of Medical Imaging, Cathay General Hospital, Taipei, Taiwan, 3Dpt of Internal Medicine, National Taiwan University Hospital, Taipei, Taiwan, 4Institute of Medical Device and Imaging, National Taiwan University, Taipei, Taiwan
Synopsis
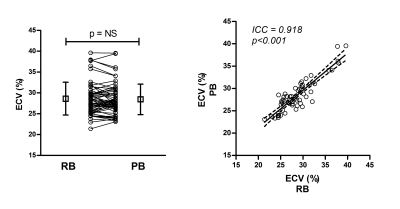
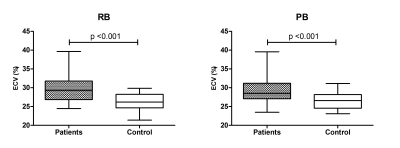
This study investigated whether free-breathing T1-acquisition with the proposed region-based (RB) method is feasible to quantify ECV as an index of diffuse myocardial fibrosis. Thirty-eight patients with non-ischemic cardiomyopathy (NICM) and 20 healthy controls were examined using both breath-hold and free-breathing myocardial T1-acquisitions. ECV was measured from free-breathing images by the RB method, which was compared with the measurement on the standard pixel-wise T1-mapping. Intraclass correlation coefficient of the two methods was 0.915. Patients with NICM showed significantly higher ECV than controls for both methods. Our results suggest that free-breathing T1-acquisition with the RB method is feasible to quantify diffuse myocardial fibrosis, and is comparable to the measurement using the standard T1-mapping.
Introduction
Measurement of myocardial T1 has been widely used to quantify the degree of diffuse myocardial fibrosis by calculating extracellular volume fraction (ECV) of the myocardium. T1 of the myocardium is most often measured by drawing a region-of-interest of the myocardium on pixel-wise T1-mapping. To obtain myocardial T1-mapping, it is necessary to acquire the images at the same cardiac phase within a single breath-hold. Poor breath-holding is known to affect the accuracy of T1 measurement despite the use of motion correction (MOCO). In this study, we proposed a region-based (RB) method which measured T1 and ECV values of a region-of-interest directly from a set of T1-mapping images acquired during free breathing. The RB method was compared with the standard pixel-based (PB) method which measured T1 and ECV pixel-wise on the T1-mapping images acquired during breath-hold. The study was conducted in patients with non-ischemic cardiomyopathy (NICM) and healthy controls. We aimed to show the proposed RB method is feasible to identify diffuse myocardial fibrosis.Methods
Thirty-eight patients with NICM and 20 healthy controls were examined on a 1.5T scanner (Aera, Siemens, Erlangen, Germany). Myocardial T1-acquisition using modified Look Locker Inversion Recovery (MOLLI) pulse sequence was implemented to acquire images under two conditions, i.e. breath-hold and shallow free-breathing. The MOLLI protocol (TR/TE/FA=1.7ms/1.1ms/35°, inversion time increment=80ms, matrix=256x192, slice thickness=8mm, spatial resolution=1.3mm and GRAPPA acceleration factor=2) used two inversion-recovery blocks to acquire 7 images for pre-contrast T1-acquisition and used three inversion-recovery blocks to acquire 8 images for post-contrast T1-acquisition. The post-contrast MOLII was performed 10 minutes after the infusion of 0.15mmole/kg of Gd-DOTA. Three short-axis planes were acquired to cover the middle zone of the left ventricle (LV). For the RB method, free-breathing images without MOCO were segmented manually in the central area of the LV cavity and the septal myocardium on each image. The averaged signal intensity of each segmented region was computed for T1 fitting. For the PB method, breath-hold images with MOCO were merged and T1-mapping was accomplished by performing the same fitting algorithm pixel-wise. The averaged T1 values of the same segmented regions as the RB method were computed. After subtracting the measurement at pre-contrast, the change of relaxation rate (1/T1) in the LV cavity and in the myocardium was obtained. The ECV values were calculated using the ratio of the change in relaxation rate in the myocardium to that in the LV cavity, and corrected for hematocrit. We averaged each ECV value over three short-axis slices for each subject. T1 and ECV values derived from the RB and PB methods were compared using paired t-test. Intraclass correlation (ICC) coefficient was used to assess the agreement between these two methods. The group comparison of ECV values between patients with controls was tested by using the Mann-Whitney U test. A value of p < 0.05 was considered significant.Results
Our results showed that T1 values measured from RB were significantly different with those measurements from PB in both myocardium (pre-contrast: 914±47ms vs. 991±37ms, p<0.001; post-contrast: 523±47ms vs. 530±53ms, p=0.019) and blood (pre-contrast: 1362±102ms vs. 1532±82ms, p<0.001; post-contrast: 411±72ms vs. 402±75ms, p<0.001). In contrast, ECV values revealed no significant difference (28.6±3.93% vs. 28.5±3.67%, p=0.491) and exhibited a strong agreement (ICC: 0.915, p<0.001) between these two methods. For group comparison, patients with NICM showed significantly higher ECV than that in the control group for both RB (29.9 ± 4.09% vs. 26.3 ± 2.24%, p < 0.001) and PB (29.5 ± 3.89% vs. 26.5 ± 2.11%, p < 0.001), respectively (Fig. 2).Discussion
High quality T1 mapping generally relies on breath-holding during image acquisition and robust MOCO processing. Respiratory motion may still occur due to diaphragmatic drift or patient’s inability or non-compliance to hold the breath. Free-breathing approach is needed for patients who are unable to adequately hold their breath, such as children and heart failure patients. Free-breathing T1-acquisition techniques have been proposed with respiratory navigator triggering or acquiring additional images with higher tissue-blood contrast to improve MOCO performance. However, residual uncorrected respiratory motion still causes errors in the pixel-wise estimation of T1-mapping. In this study, we proposed an alternative region-based approach to generate a single T1 value on free-breathing images. Although T1 values were significantly different between the two methods, ECV values were not significantly different. Group comparison showed that ECV measurement from the RB method was able to differentiate the myocardial abnormalities as was the PB method.Conclusion
Free-breathing T1-acquisition with the RB method is feasible to quantify diffuse myocardial fibrosis as compared with the measurement with standard T1-mapping.Acknowledgements
This work was supported by the Ministry of Science and Technology, Taiwan (grants MOST 106-2314-B-002-068).References
- Su MY, Lin LY, Tseng YH, et al. CMR-verified diffuse myocardial fibrosis is associated with diastolic dysfunction in HFpEF. JACC Cardiovasc Imaging. 2014;7(10):991-7.
- Mehta BB, Chen X, Bilchick KC, et al. Accelerated and navigator-gated look-locker imaging for cardiac T1 estimation (ANGIE): Development and application to T1 mapping of the right ventricle.Magn Reson Med. 2015;73(1):150-60.
- Chow K, Yang Y, Shaw P, et al.Robust free-breathing SASHA T1 mapping with high-contrast image registration.J Cardiovasc Magn Reson. 2016;18(1):47.
Figures