4875
Elevated NT-proBNP in a Community Cohort is Associated with Myocardial Fibrosis: the Multi-Ethnic Study of Atherosclerosis (MESA)Chia-Ying Liu1, Susan R Heckbert2, Shenghan Lai3, Bharath Amable-Venkatesh4, Mohammad R Ostovaneh4, Robyn L McClelland5, Joao A.C Lima4, and David A Bluemke6
1Radiology and Imaging Sciences, National Institutes of Health, Bethesda, MD, United States, 2Department of Epidemiology, University of Washington, Seattle, WA, United States, 3Department of Pathology, Johns Hopkins School of Medicine, Baltimore, MD, United States, 4Department of Radiology, Johns Hopkins School of Medicine, Baltimore, MD, United States, 5Department of Biostatistics, University of Washington, Seattle, WA, United States, 6David Bluemke, University of Wisconsin, Madison, WI, United States
Synopsis
We evaluated the relationship between cardiac MRI measures of fibrosis and NT-proBNP levels in 1334 participants in the Multi-Ethnic Study of Atherosclerosis (MESA). Univariate and multivariable regression analyses adjusting for demographics, cardiovascular risk factors, and left ventricular (LV) mass were performed to examine the association of log NT-proBNP with MRI T1 mapping indices. In the fully adjusted model, each one standard deviation increment (0.44pg/mL) of log NT-proBNP was associated with 0.62% increment in ECV (P<0.001), 4.7ms increment in native T1 (P=0.001), and 0.01 increment in partition coefficient (P<0.001). Elevated NT-proBNP is related to subclinical fibrosis in a community-based setting.
Background
Serum N-terminal proB-type natriuretic peptide (NT-proBNP) is considered a marker that is expressed in response to myocardial strain and possibly fibrosis. However, the relationship to myocardial fibrosis in a community-based population is unknown. We evaluated the relationship between cardiac MRI measures of fibrosis and NT-proBNP levels in the Multi-Ethnic Study of Atherosclerosis (MESA).Methods
A total of 1334 participants (52% white, 23% black, 11% Chinese, 14% Hispanic, 52% men with mean age 67.6 years) at six sites had both serum NT-proBNP measurements and cardiac MRI with T1 mapping indices of fibrosis at 1.5 Tesla. T1 mapping indices including pre (native) and post-contrast T1 times at 12 and 25 minutes, partition coefficient (l), and extracellular volume fraction [ECV=100´l´(1-hematocrit)] were assessed using a single-breath hold modified Look-Locker inversion recovery (MOLLI) sequence. Linear regression was used to determine the relationship between log10 NT-proBNP and each T1 index. Regression models were examined as follows: Unadjusted models were fit, followed by models minimally adjusted for age, gender, and race, and finally fully adjusted models including minimal + smoking status, body mass index, heart rate, systolic blood pressure, diastolic blood pressure, LDL-c, HDL-c, triglyceride, hypertension (including those with antihypertensive treatment), diabetes, serum creatinine, statins usage, cardiovascular events, and LV mass.Results
Characteristics of the study cohort are shown in Table 1. Figure 1 demonstrates the box plot of log (NT-proBNP) across quartiles of ECV. Table 2 shows the relationship of MRI markers of myocardial fibrosis and log NT-proBNP. In the regression analyses, log NT-proBNP was positively associated with all markers in the unadjusted analyses (all P<0.001). However, the associations only remained significant in ECV, (B=1.4, P<0.001), partition coefficient (B=0.024, P<0.001), and native T1 (B=10.66, P=0.001) in the fully adjusted model. Post T1 times were not associated with NT-proBNP levels after adjustments. The unadjusted associations of ECV, native T1, and post contrast T1 times at 12 minutes with log NT-proBNP are presented in Figure 2. Table 3 further displays standardized results for the association of ECV, partition coefficient, and native T1 with log NT-proBNP in the fully adjusted model, in which a 1-SD increment of log NT-proBNP (0.44 pg/mL) was associated with increments of 0.62% in ECV, 0.01 in partition coefficient, and 4.72 ms in native T1. Adjusting further for confounders including educational level, physical activity, or coronary calcium score also did not substantially alter the results. ECV appeared strongly associated with log NT-proBNP regardless of the covariates.Discussion
In a large community-based population, we demonstrated a positive relationship between an imaging biomarker for diffuse fibrosis (MRI ECV) and an established serum biomarker (NT-proBNP) for heart failure. Our results suggest that NT-proBNP identifies a subclinical pro-fibrotic in a community population. Further clarification will importantly assist in understanding the significance and utility of these biomarkers in studying the pathogenesis of fibrosis in heart failure.Acknowledgements
The authors thank all investigators, staff, and participants of the MESA Study for their valuable contributions. A full list of participating MESA Investigators and institutions can be found at http://www.mesa-nhlbi.org. This research was supported by contracts HHSN268201500003I, N01-HC-95159, N01-HC-95160, N01-HC-95161, N01-HC-95162, N01-HC-95163, N01-HC-95164, N01-HC-95165, N01-HC-95166, N01-HC-95167, N01-HC-95168 and N01-HC-95169 from the National Heart, Lung, and Blood Institute, and by grant R01 HL127659.References
No reference found.Figures
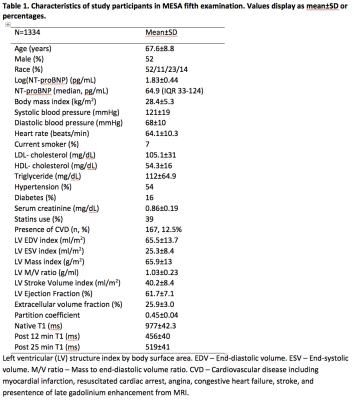
Table 1
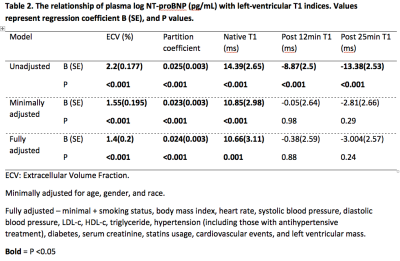
Table 2
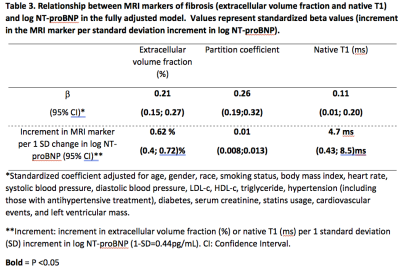
Table 3
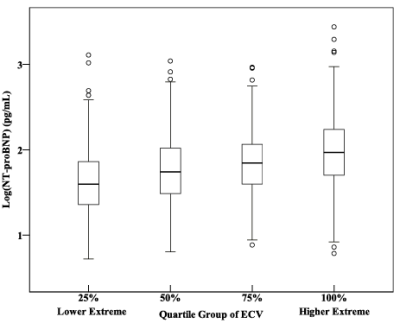
Figure 1. Box plot of log NT-proBNP across quartiles
of MRI extracellular volume fraction (ECV).
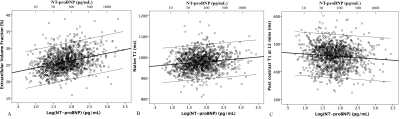
Figure 2. The unadjusted relationships between log
NT-proBNP and T1 indices.
The relationships between log NT-proBNP and myocardial
fibrosis assessed by MRI extracellular volume fraction (ECV) (A), native T1
(B), and post contrast T1 at 12 minutes (C).