4848
Radiological Assessment of Vascular Supply of Intracranial Meningeomas by Superselective Arterial Spin Labelling.1University Hospital Center of Schleswig-Holstein, Campus Kiel, Department of Radiology and Neuroradiology, Kiel, Germany, 2Philips Research, Hamburg, Germany, 3University Hospital Center of Schleswig-Holstein, Campus Kiel, Department of Neurosurgery, Kiel, Germany
Synopsis
Detailed information on the extent and ratio of blood supply is required to assess the feasibility of presurgical embolisation procedures of intracranial meningeomas. This study investigates the feeding vasculature to intracranial meningeomas using superselective ASL. In 31 prospectively included patients harboring a total of 42 meningeomas, superselective ASL was performed to visualize the contribution of blood supply to the tumor and rated by two readers. We demonstrated that superselective ASL is capable of identifying and quantifying the contribution of feeding arteries in intracranial meningeomas. Agreement with gold standard DSA is also demonstrated.
Introduction
Meningeomas are the most common benign tumors of the central nervous system. If surgical removement is required, presurgical embolisation may be useful in selected cases to reduce bleeding complications. Detailed information on the extent and ratio of blood supply from the external and internal carotid artery is required to assess the feasibility of embolisation procedures. This is usually obtained by digital subtraction angiography (DSA). However, DSA is an invasive procedure utilizing ionizing radiation and bears the risk of stroke, hemorrhage and reactions to the iodinated contrast agent. Typical MRI based perfusion and angiographic techniques like dynamic susceptibility contrast (DSC) MRI or Time-of-Flight (TOF) angiography are non-selective and cannot differentiate the contribution of multiple feeding vessels. Recently, superselective Arterial Spin Labeling (ASL) has been introduced that overcomes such limitations and makes it possible to selectively label blood of individual cerebral arteries1. This study investigates the feeding vasculature to intracranial meningeomas. Superselective ASL was used to identify and quantify the contribution of blood supply of individual supplying vessels to the tumors.
Material and Methods
In 31 prospectively included patients (28 females, 3 males), harboring a total of 42 intracranial meningeomas (median 1, range 1-7), superselective ASL was performed to visualize the contribution of blood supply to the tumors for both internal carotid arteries (ICA), vertebral arteries (VA), and external carotid arteries (ECA). All measurements were performed on a clinical Philips 3 Tesla Achieva scanner (Philips, Best/The Netherlands) using the following parameters: FOV 220 x 220 x 104 mm3, voxel size of 2.7 x 2.7 x 6 mm3, gradient echo planar read-out, labeling duration 1.65 s, postlabeling delay 1.525 s with background suppression, 15 slices and 20 averages of label and control images. Scan time was approximately 2:40 min per vessel. The perfusion-weighted images were used for subsequent rating. For anatomical delineation of the tumor contrast-enhanced T1-weighted images were available in all cases. Two readers independently rated the presence and extent of blood supply to the tumor for each labeled vessel (“<50%”, “>50%” or “no supply”)2. If disagreement was present, a consensus was reached after discussion in a consensus session. Interrater agreement was calulated using Cohen‘s 𝛞. Validation was performed in one patient receiving DSA and presurgical embolisation.Results
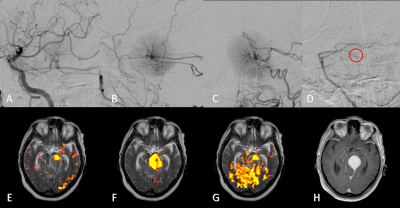
Superselective ASL was technically successful in all cases. Interrater agreement was 0.68. 47% of the tumors exhibited mixed vascular contribution from multiple vessels. 33% of the tumors had bilateral vessel supply. The agreement between ASL and DSA is demonstrated in Fig. 1. The identification of the extent of the tumors was not a main source of disagreement between raters. If disagreement between raters was present the following reasons could be identified: 1) Small size of the tumor 2) Insufficient signal to noise ratio in the ASL images to differentiate between tumor and vessel 3) Atypical tumors with necrosis.Discussion
We demonstrated that selective ASL is capable of identifying and quantifying the contribution of feeding arteries in intracranial meningeomas. Agreement with gold standard DSA was demonstrated. In contrast to DSA this technique is completely non invasive, works without contrast agent and ionizing radiation and is thus repeatable without hazards. Details on tumor vascularisation may be useful in planning presurcgical embolisation. The obtained information may also be used to plan the surgical approach and to mitigate intraoperative bleeding. Using this technique, en passant feeders simultaneously supplying tumor and cerebral tissue may be identified. Further, it has the potential to aid the diagnosis between intra- and extraaxial tumors.Acknowledgements
No acknowledgement found.References
1: Helle M, Norris DG, Rüfer S, et al. Superselective pseudocontinuous arterial spin labeling. Magn Reson Med. 2010;64(3):777-86.
2: Nania A, Granata F, Vinci S, et al. Necrosis score, surgical time, and transfused blood volume in patients treated with preoperative embolization of intracranial meningiomas. Analysis of a single-centre experience and a review of literature. Clin Neuroradiol. 2014;24(1):29-36.
Figures