4841
Association between Diffusion Weighed Imaging Measured Pretreatment Ischemic Volume and Functional Outcome in Ischemic Stroke1IADI, U947, INSERM, Université de Lorraine, CHRU Nancy, Nancy, France, 2Department of Neuroradiology, Sainte-Anne Hospital and Paris-Descartes University, INSERM U894, Paris, France, 3CIC 1433 Epidémiologie Clinique, INSERM, Université de Lorraine, CHRU Nancy, Nancy, France, 4INSERM U1237, “Physiopathology and Imaging for Neurological Disorders (PhIND)”, GIP Cyceron, Caen, France, 5Department of Neuroradiology, University Hospital of Rennes, Rennes, France, 6Department of Neuroradiology, University Hospital of Reims, Reims, France, 7CIC 1433 Innovation Technologique, INSERM, Université de Lorraine, CHRU Nancy, Nancy, France, 8Department of Diagnostic and Interventional Neuroradiology, CHRU Nancy, Nancy, France
Synopsis
The association between pretreatment ischemic volume (PIV) measured on diffusion weighted images (DWI) and functional outcome after mechanical thrombectomy is of great clinical importance but has yet to be determined. We analyzed 298 ischemic stroke patients from the multicentric study THRACE. Our results showed that increased PIV was an independent predictor for a lower probability of functional independence, a less favorable degree of disability, and a higher mortality rate. PIV measured on DWI is a valuable early predictor for functional outcome in ischemic stroke patients, and thus can contribute to patient selection for optimal therapeutic intervention.
Introduction
Recent randomized clinical trials have demonstrated the clinical benefit of mechanical thrombectomy in acute ischemic stroke patients with anterior circulation proximal intracranial occlusions.1 In the majority of these trials, patients were evaluated with computed tomography (CT). A large pretreatment ischemic core volume (usually determined visually) was an exclusion criterion as it was considered that the clinical benefit would be little under this circumstance. However, CT may inappropriately depict ischemic volume due to its poor contrast between ischemic regions and normal regions. Diffusion-weighted imaging (DWI) has been demonstrated to be more helpful for ischemic core evaluation.2 Nevertheless, the association between pretreatment ischemic volume (PIV) measured on DWI (DWI-PIV) and functional outcome after mechanical thrombectomy has yet to be determined. In this study, we aimed to characterize the relationship between DWI-PIV and the functional outcome in ischemic stroke patients.Methods
Patients: 298 anterior circulation ischemic stroke patients who had pretreatment DWI were included in this work. They were all recruited in a multicentric study THRACE3, which was a randomized controlled trial done in 26 centers in France, comparing intravenous thrombolysis plus mechanical thrombectomy (IVTMT) and intravenous thrombolysis alone (IVT) in acute ischemic stroke patients. It provides a unique opportunity to investigate the DWI-PIV, because of the use of DWI in pretreatment imaging in a large proportion of patients and the absence of exclusion criteria on the basis of PIV.
Data analysis: Pretreatment lesion regions were semi-automatically segmented after applying a threshold of apparent diffusion coefficient (ADC) of 0.6×10-3 mm2/s on ADC maps, which were reconstructed from DWI acquisitions. DWI-PIVs were automatically measured based on the delineated lesion regions. All the analyses were performed using Olea Sphere® (Olea Medical SAS, La Ciotat, France).
Outcome assessment and statistical analysis: Primary outcome was the proportion of patients achieving functional independence at 3 months, defined by the modified Rankin Scale (mRS) 0-2. Secondary outcomes were (1) degree of disability at 3 months, assessed by the ordinal mRS from 0 to 6 with ranks 5 and 6 combined into a single category; and (2) mortality at 3 months. Logistic regression was applied to model clinical outcome as a function of DWI-PIV. α=0.05 was chosen as the significance level, statistical analyses were performed using statistical software R (version 3.3.2)
Results
Of 298 patients, with median ischemic volume 17.2 mL (interquartile range [IQR] 9.2-51.8) and median mRS 2 (IQR 1-4), 51.0% achieved functional independence.
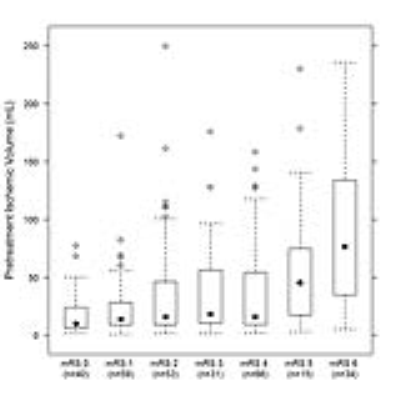
The distribution of DWI-PIV for each mRS level is shown in Figure 1. Increased ordinal mRS was associated with a larger DWI-PIV (Spearman’s ρ correlation coefficient 0.34; p<0.0001). Increased DWI-PIV was an independent predictor for a lower probability of functional independence (odds ratio [OR] 0.90 [95% confidence interval [CI] 0.81-0.99] per 10 mL, p<0.001), a less favorable degree of disability (common OR [cOR] 0.86 [95% CI 0.81-0.90] per 10 mL, p<0.001), and a higher mortality rate (OR 1.21 [95% CI 1.08-1.37] per 10 mL, p<0.001). The associations between DWI-PIV, age, baseline NIHSS score, and adjusted probability of functional independence were depicted by three-dimensional scatterplots with fitted surfaces (Fig 2). No significant treatment-by-dichotomized DWI-PIV (dichotomized by PIV of 70 mL and 100 mL) interaction for functional independence was observed.
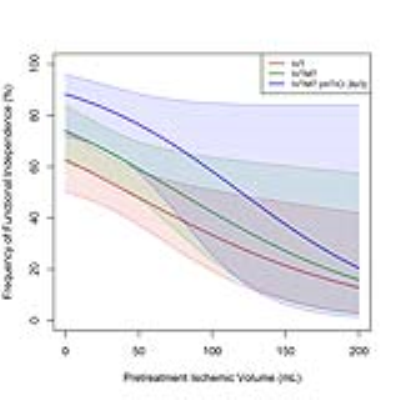
With the increase of DWI-PIV, the probability of achieving functional independence decreased in both the IVTMT group and the IVT group (Fig 3). For the IVTMT group patients: OR 0.87 (95% CI 0.77-0.98, p=0.02) per 10 mL; for the IVT group patients: OR 0.89 (95% CI 0.80-0.97, p=0.01) per 10 mL; for the IVTMT group patients with substantial reperfusion (defined as a modified Thrombolysis in Cerebral Infarction (mTICI) scale score of 2b or 3): OR 1.26 (95% CI 1.00-1.59, p=0.04) per 10 mL.
Discussion
Our results demonstrated that DWI-PIV was an independent predictor for functional disability and mortality. The nonsignificant treatment-by-dichotomized DWI-PIV interaction for clinical outcome suggested that excluding patients based on a simple DWI-PIV threshold would be unadvisable. Besides, we confirmed the importance of substantial reperfusion for a favorable functional outcome, as previously reported elsewhere.4Conclusion
DWI-PIV is a valuable early predictor for functional outcome in ischemic stroke patients, and thus can contribute to patient selection for optimal therapeutic intervention.Acknowledgements
We thank Farhat Benbelkacem and Raphaël Petazzoni (Olea Medical) for their help in image postprocessing.
References
1. Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387(10029):1723-1731.
2. Edlow, J. A. Evidence-based guideline: the role of diffusion and perfusion MRI for the diagnosis of acute ischemic stroke: report of the Therapeutics and Technology Subcommittee of the American Academy of Neurology. Neurology. 2011;76(23):177-185.
3. Bracard S, Ducrocq X, Mas JL, et al. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol. 2016;15(11):1138-1147.
4. Gilgen MD, Klimek D, Liesirova KT, et al. Younger Stroke Patients With Large Pretreatment Diffusion-Weighted Imaging Lesions May Benefit From Endovascular Treatment. Stroke. 2015;46(9):2510-2516.
Figures