4837
Evaluation of Tranvascular Water Exchange Index (WEI) in post Thrombectomy PatientsYoung Ro Kim1 and Jerold L. Boxerman2
1Radiology, Martinos Center for Biomedical Imaging MGH/HMS, Charlestown, MA, United States, 2Diagnostic Imaging, Rhode Island Hospital and Warren Alpert Medical School of Brown University, Providence, RI, United States
Synopsis
The dynamic evolution of vascular impairment following thrombotic stroke has important clinical implications for designing effective management and treatment strategies. In the current study, we quantified the rate of water exchange across the blood-brain barrier (BBB) via water exchange index (WEI) in clinical patients undergone thrombectomy. Although extravasation of Gd-DTPA was not observed in most of the patients, the WEI was significantly elevated in both infarct and peri-infarct areas, revealing compromised integrity of the BBB.
Introduction
Thrombotic stroke often exhibits abnormal displacement of tissue water at both cellular and tissue levels. At an acute stage of stroke, cell swelling and restricted water diffusion develop while vascular water accumulates in the interstitial space at later phases, via mechanisms of cytotoxic and vasogenic edema, respectively. Although limited by the time window and complications, clinical options for treating thrombosis have been effective at acute stages with (i) thrombolysis using tissue plasminogen activator (tPA) and (ii) mechanical thrombectomy using a catheter to reestablish blood flow to the parts of the brain being deprived of blood supply. However, the grave clinical implications of hemorrhagic transformation and malignant cerebral edema caused by vasogenic edema, due to the dysfunctional blood-brain barrier (BBB) still pose as threats to the treated patients. Typical clinical assessment of BBB damage using dynamic contrast enhanced (DCE) MRI method relies heavily on the extravasation of Gd-DTPA (547 Da) to characterize the post stroke BBB breakdown. Therefore, the evaluation of damaged but non-leaky BBB has been difficult. To address such methodological shortcoming, we quantified water exchange index (i.e., rate of water movement across the BBB) in the post thrombectomy patients who did not display any leaks to Gd-DTPA.Methods
Thrombotic stroke patients (N = 6) who underwent thrombectomy were imaged in a 3T clinical scanner (Trio; Siemens) before and after Gd-DTPA injection using flow-compensated 3D multi gradient with TR=40ms, 8 echoes at TE=[1.41, 4.41, 7.41, 10.41, 13.41, 16.41, 19.41, 22.41], matrix=256x256, FOV=266mm and flip angles at 30 and 80, resulting in total scan time of ~ 2 min for each flip angle acquisition. As described previously,1 water exchange index (WEI) was calculated in the infarct ROI defined by ADC (25% lower than contralesional counter part) and peri-infacrt areas.2Results
The water exchange index (WEI: which is largely proportional to the actual water exchange rate) was successfully quantified in human stroke patients who did not display extravasation of Gd-DTPA. For ROI’s defined by the reduced ADC (see Figure 1), the average WEI was significantly elevated compared to the contralesional counterpart (Figure 2). However, upon inspection, two patients did not show increased WEI in the ADC-defined lesion areas despite the apparent infarct and associated MRI traits (see Figure 1), revealing minimal deterioration in the BBB integrity. No significant correlation was found between ADC and WEI.Discussion
Following thrombectomy, even for the brains that did not display apparent vascular wall damage (i.e., lack of leaky vessels in DCE MRI), the WEI values were generally elevated in both infarct and infarct periphery. The findings show that the WEI is a sensitive biomarker, capable of assessing subtle changes in the BBB integrity and may be used at early stages of BBB deterioration to predict the vascular outcome after stroke. The current study also demonstrates feasibility of the WEI acquisition in a clinical setting with an additionally required scan time of less than 10 minutes. The variable WEI results among subjects warrant follow-up studies of the patients undergone thrombolysis or thrombectomy to investigate how the WEI values are related with the stroke outcome.Conclusion
Quantification of water exchange rate across the BBB provides an effective means to assess subtle changes in stroke patients before the barrier function of the BBB is overtly compromised.Acknowledgements
No acknowledgement found.References
- Huang S. Dynamic Monitoring of Blood-Brain Barrier Integrity using Water Exchange Index (WEI) During Mannitol and CO2 Challenges in Mouse Brain. NMR in Biomedicince. 2013 April;26(4) 376-385.
- Huang S. Cerebral blood volume affects blood-brain barrier integrity in an acute transient stroke model. J Cereb Blood Flow Metab. 2013 Jun;33(6):898-905
Figures
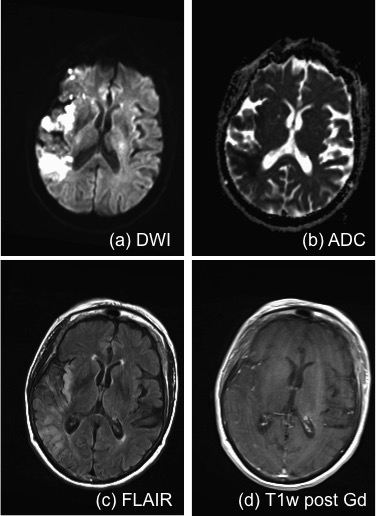
Figure 1. Representative MRI of
thrombotic stroke patients undergone thrombectomy: despite the apparent lesion,
there was no extravasation of Gd-DTPA.
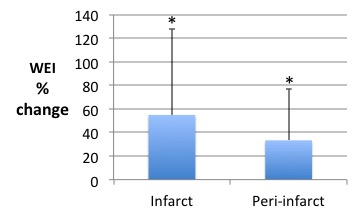
Figure 2. Elevated water Exchange
Index (WEI) in infarct and peri-infarct areas: WEI was normalized to that
measured in the contralesional counterpart.