4833
Predicting Hyperperfusion syndrome by measurement of leptomenigeal collateral and preoperative cerebral blood flow in patients with unilateral internal carotid artery stenosis1Radiology and Imaging, Chinese People’s Liberation Army (PLA) General Hospital, Beijing, China, 2General Electric Healthcare, Shang hai, China
Synopsis
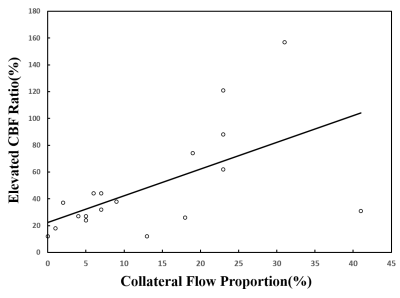
Hyperperfusion syndrome (HPS) is a rare but potentially fatal postoperative complication after revascularization, while preoperative predictor of HPS had not been fully established. We used pseudo continuous arterial spin labeling (pCASL) to investigate the correlation between the collateral flow proportion and the elevated cerebral blood flow (CBF) ratio relative to the preoperative CBF in patients with unilateral internal carotid artery (ICA) stenosis. A significant correlation was observed between the collateral flow proportion and the elevated CBF ratio . (r =0.588, P =0 .01). As an indication, HPS are likely to occur in patients with low preoperative CBF and good collateralization.
Introduction
Hyperperfusion syndrome (HPS) is a rare but potentially fatal postoperative complication after carotid artery stenting (CAS) and endarterectomy (CEA)1. Hence a preoperative predictor of HPS has great clinical value. Previous work had shown that deficient collateralization may be a potential indicator for intracranial HPS2; a recent study also suggested leptomeningeal collaterals as a major risk factor3. A potential reason for the discrepancy in previous reports is the individual differences, which may lead to over or under-estimate of collateralization relative to preoperative cerebral blood flow (CBF). In our study, the preoperative CBF was used as a reference to eliminate the potential difference. The purpose of this study was to investigate the correlation between the collateral flow proportion and the elevated CBF ratio, in the hope of providing a prognosis index for HPS.Method
Eighteen patients (15 males and 3 females; age=61.6±8.2 years) with 70%-99% unilateral stenosis in internal carotid artery were prospectively and consecutively enrolled as confirmed by conventional angiography and underwent either CAS (n=11) or CEA (n=7) from November 2015 to February 2017. All patients received MR exams including routine sequences, 3D T1-FSPGR, and 3D ASL (post labeling delay 1.5, 2.0, and 2.5s) within 7 days prior to CAS and CEA, and then 24h, 48h, 72h, and 96h post CEA and CAS on a 3.0T whole body scanner (Discovery MR750, GE). Blood pressure was kept 110-120/70-80mmHg for patients during 24-96h after operation. A volumetric internal carotid artery territory based on gray matter mask according to previous work was used to measure mean CBF value of ipsilateral and contralateral side4,5. Late-arriving retrograde flow representing collateral flow was calculated through previous method reported in the literature, which was defined as [CBF2.5 s−CBF1.5 s] at lesion side − [CBF2.5 s−CBF1.5 s] at normal side6. The elevated CBF values at lesion side were obtained as (highest CBF2.0s 24-96h post-operation) - (preoperative CBF2.0s). The collateral perfusion proportion was defined as (collateral flow) / (preoperative CBF2.0s). The elevated CBF ratio was defined as (elevated CBF) / (preoperative CBF2.0s). Spearman correlation coefficients between the collateral flow proportion and the elevated ratio was analyzed.Results
The CBFs of eighteen patients were listed in Table 1.The collateral flow proportion and the elevated ratio were listed in Table 2. A significant correlation was observed between the collateral flow proportion and the elevated CBF ratio. (r =0.588, P =0 .01) (Figure 1).Discussion and conclusion
In this work, elevated CBF ratio was observed to correlate with collateral flow proportion: the higher collateral flow proportion, the higher elevated CBF ratio. The higher collateral flow proportion included two categories: preoperative hypoperfusion and the higher collateral flow; and relatively high preoperative CBF and even higher collateral flow. However, patients with greater perfusion deficits prior to operation have greater improvement in perfusion after operation7. Thus, we should pay more attention to the first category. As an indication, HPS are likely to occur in patients with low preoperative CBF and good collateralization.Acknowledgements
We thank all the subjects for participating in the study.References
1.Ziaja D, Biolik G, Kocełak P, et al. Neurological symptoms associated with cerebral hyperperfusion syndrome after CEA and CAS--one centre study.[J]. Eur Rev Med Pharmacol Sci, 2014, 18(8):1176-80. 2. Xu S, Pei W, Shi H, et al. Hyperperfusion Syndrome After Stenting for Intracranial Artery Stenosis[J]. Cell Biochemistry & Biophysics, 2014, 71(3):1-6. 3. Lee K J, Kwak H S, Chung G H, et al. Leptomeningeal collateral vessels are a major risk factor for intracranial hemorrhage after carotid stenting in patients with carotid atherosclerotic plaque.[J]. Journal of Neurointerventional Surgery, 2015. 4.Nowinski W L, Qian G, Kirgaval Nagaraja B P, et al. Analysis of Ischemic Stroke MR Images by Means of Brain Atlases of Anatomy and Blood Supply Territories[J]. Academic Radiology, 2006, 13(8):1025-34. 5. Lee J S, Lee D S, Kim Y K, et al. Probabilistic map of blood flow distribution in the brain from the internal carotid artery.[J]. Neuroimage, 2004, 23(4):1422-1431. 6.Lyu J, Ma N, Liebeskind D S, et al. Arterial Spin Labeling Magnetic Resonance Imaging Estimation of Antegrade and Collateral Flow in Unilateral Middle Cerebral Artery Stenosis[J]. Stroke; a journal of cerebral circulation, 2016, 47(2):428. 7. Yun T J, Sohn C H, Han M H, et al. Effect of carotid artery stenting on cerebral blood flow: evaluation of hemodynamic changes using arterial spin labeling[J]. Neuroradiology, 2013, 55(3):271-81.Figures
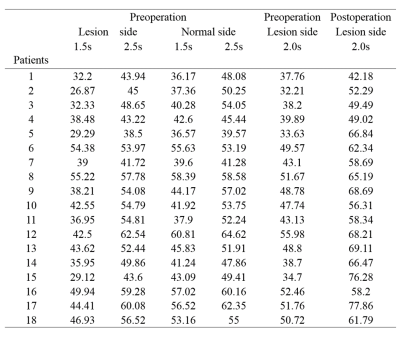
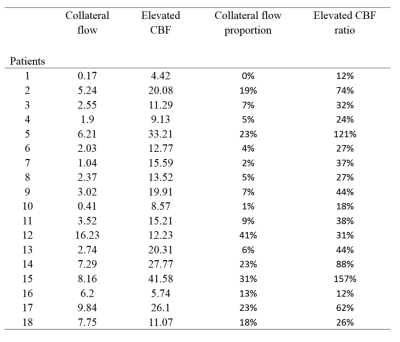
Table2. Eighteen patients’ collateral flow, elevated CBF, collateral flow proportion and elevated CBF ratio in internal carotid artery territory. CBF indicates cerebral blood flow.
Collateral flow= [CBF2.5 s−CBF 1.5 s] at lesion side−[CBF 2.5 s−CBF 1.5 s] at normal side.
Elevated CBF= Postoperative CBF2.0s-Preoperative CBF2.0s
Collateral flow proportion=Collateral flow/ Preoperative CBF2.0s
Elevated CBF ratio= Elevated CBF/ Preoperative CBF2.0s