4831
Proximal Internal Carotid Artery Stenosis Associates with Diffuse Wall Thickening in Petrous Arterial Segment of Moyamoya Disease Patients: A 3D MR Vessel Wall Imaging Study1Center for Brain Disorders Research, Capital Medical University, Beijing, China, 2Center for Biomedical Imaging Research, Tsinghua University, Beijing, China, 3Department of Neurosurgery, Affiliated Drum Tower Hospital of Nanjing University Medical School, Nanjing, China, 4Department of Radiology, Affiliated Drum Tower Hospital of Nanjing University Medical School, Nanjing, China
Synopsis
It has been shown that rapid reduction of lumen diameter at the proximal ICA can be seen in moyamoya disease (MMD) patients. The arterial wall thickness at downstream of proximal ICA may aggravate cerebral ischemia and affect the outcome of revascularization. This study sought to investigate the association between proximal ICA stenosis and diffuse wall thickening in ipsilateral petrous ICA in MMD patients. We found that proximal ICA stenosis was significantly associated with wall thickness (r = 0.434, p<0.001) and presence of diffuse wall thickening (odds ratio=4.433, 95% confidence interval 1.980–9.925, p<0.001) in ipsilateral petrous ICA in MMD patients.
Introduction
Moyamoya disease (MMD) is a cerebrovascular disorder which not only involves the intracranial arteries but also affects extracranial carotid arteries. 1,2 It has been shown that rapid reduction of the diameter at the proximal portion of extracranial internal carotid artery (ICA) can occur in a substantial number of MMD patients. 3-5 Previous study reported that patients with severe carotid atherosclerotic stenosis had diffuse wall thickening (DWT) in ipsilateral petrous ICA which may affect the efficiency of revascularization treatment. 6 However, it is unknown whether the DWT can be detected in petrous ICA in MMD patients with severe stenosis in proximal ICA. This study sought to investigate the association between proximal ICA stenosis and DWT in ipsilateral petrous ICA in MMD patients.Methods
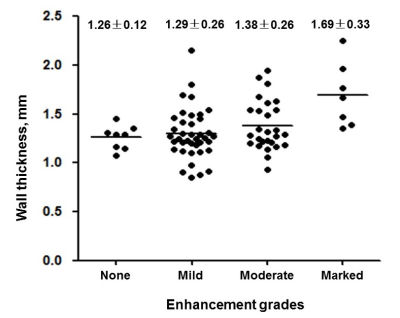
Study sample: Forty-one with confirmed MMD subjects (mean age 42.8±11.0 years, 19 males) were recruited and underwent MR vessel wall imaging for carotid arteries. The study protocol was approved by institutional review board and written consent form was obtained from each patient. MR imaging: MR imaging was conducted on a 3.0T MR scanner with a 16-channel phased array head-neck coil. The carotid MR imaging protocol and parameters are as follows: 3D time-of-flight (TOF): TR/TE 25/3.5 ms, 20°, field of view (FOV) 18x18x6 cm3, spatial resolution 1.0 mm3; pre- and post-contrast 3D T1-VISTA: TR/TE 800/19 ms, flip angle 90°, field of view (FOV) 20x18x4 cm3, spatial resolution 0.5 mm3. Gadolinium contrast agent was administrated intravenously with 0.1 mmol/kg for post-contrast scan. Data analysis: All images were reviewed by two experienced radiologists with consensus. The diameter of ICA and common carotid artery (CCA) were measured on 3D TOF MRA images. The stenosis of proximal ICA was calculated by the formula: (1- ICA diameter/CCA diameter) ×100%. The wall thickness (WT) of the petrous ICA was measured on T1-VISTA images. DWT of petrous ICA was identified as mean WT>1.5mm. The enhancement degree of petrous ICA was recorded and graded into 4 grades (none to marked) on the CE-T1-VISTA images. Statistical analysis: The association between stenosis of proximal ICA and wall thickness and presence of DWT in petrous ICA were determined using Pearson correlation and logistic regression analyses. The wall thickness and presence of DWT in petrous ICA were compared among different enhancement grades using non-parametric Kruskal-Wallis test.Results
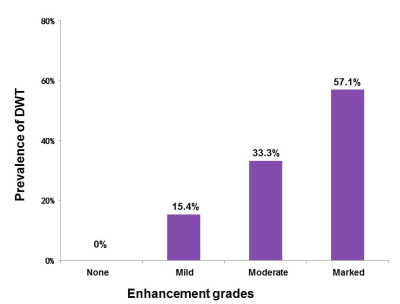
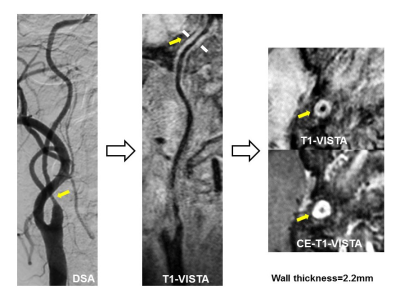
In total, 81 arteries from 41 patients were included in the final statistical analysis. Pearson correlation analysis showed that the proximal ICA stenosis was significantly correlated with the wall thickness in petrous ICA (r = 0.434, p<0.001). Logistic regression analysis revealed that the odds ratio (OR) of the proximal ICA stenosis with increment of 10% was 3.731 (95% confidence interval [CI] 1.725–6.585, p<0.001) in discriminating the presence of DWT of petrous ICA. After adjusting for confounding factors, the association was still statistically significant (OR=4.433, 95% CI 1.980–9.925, p<0.001). An increasing trend was found in prevalence of DWT (p=0.022, Fig. 1) and WT (p=0.11, Fig. 2) with enhancement grades in petrous ICA. Fig. 3 represents an example with significant stenosis in proximal ICA and DWT in petrous ICA at the same patient.Discussion and Conclusion
The proximal ICA stenosis was significantly associated with wall thickness and diffuse wall thickening in ipsilateral petrous ICA in MMD patients. Similar phenomenon has been reported in patients with severe carotid atherosclerotic stenosis. 6 In the present study, the diffuse wall thickening and wall enhancement could be explained by the pathophysiological processes of ischemia injury and the inflammation reaction due to severe proximal ICA stenosis. However, the natural history and the sequelae of diffuse wall thickening in petrous ICA among MMD subjects is not clear and needs to be prospectively studied.Acknowledgements
None.References
1. Suzuki J, Takaku A. Cerebrovascular “Moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol. 1969;20:288-299.
2. Yang SH, Li B, Wang CC, et al. Angiographic study of Moyamoya disease and histological study in the external carotid artery system. Clin Neurol Neurosurg. 1997;99:S61–S63.
3. Yasaka M, Ogata T, Yasumori K, et al. Bottle neck sign of the proximal portion of the internal carotid artery in Moyamoya disease. J Ultrasound Med. 2006;25:1547–1552.
4. Shimogawa T, Morioka T, Sayama T, et al. Champagne bottle neck sign in a patient with Moyamoya syndrome. World J Clin Cases. 2014;2:474-477.
5. Yasuda C, Arakawa S, Shimogawa T, et al. Clinical Significance of the Champagne Bottle Neck Sign in the Extracranial Carotid Arteries of Patients with Moyamoya Disease. AJNR Am J Neuroradiol. 2016 May 26.
6. Chen X, Zhao H, Chen Z, et al. Association between proximal internal carotid artery steno-occlusive disease and diffuse wall thickening in its petrous segment: a magnetic resonance vessel wall imaging study. Neuroradiology. 2017;9: 485-490.
Figures