4830
Vessel Encoded Arterial Spin Labeling Evaluation of Collateral Circulation in Symptomatic and Asymptomatic Patients with Internal Carotid Artery or Middle Cerebral Artery Occlusion1Department of Radiology, Chinese PLA General Hospital, Beijing, China
Synopsis
Symptomatic and asymptomatic patients with internal carotid artery (ICA) or middle cerebral artery (MCA) occlusion have the different prognosis. The present study had evaluated collateral circulation by Vessel Encoded Arterial Spin Labeling (VE-ASL) and cerebral vasoreactivity by mean transit time (MTT) obtained by Dynamic susceptibility contrast in symptomatic and asymptomatic patients with unilateral ICA and/or MCA occlusion. The study had found that the intensity of collateral in asymptomatic patients was significantly better than symptomatic patients while MTT showed no significant differences, which indicate that hemodynamic impairments in symptomatic patients with ICA/MCA occlusion may be mainly induced by the insufficiency of collateral circulation.
Introduction
Symptomatic and asymptomatic patients with internal carotid artery (ICA) or middle cerebral artery (MCA) occlusion have the different prognosis. The symptomatic patients had a higher recurrent stroke than that of asymptomatic patients. The important factors determining the disease evolution include collateral circulation, cerebral vasoreactivity, and etiology of occlusion. Asymptomatic occlusion was considered as the benign condition, differences between symptomatic and asymptomatic occlusion regarding the disease evolution determinants remain unclear, but which is helpful to understanding the mechanism of stroke resulting from artery occlusion and improve patients management. The aim of the study was to evaluate collateral circulation and cerebral vasoreactivity in symptomatic and asymptomatic patients with unilateral ICA and/or middle MCA occlusion.Methods
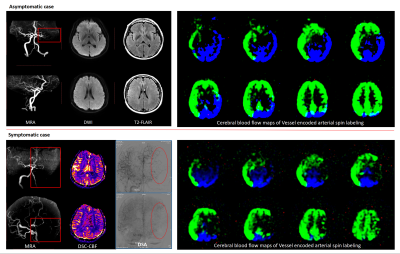
In the retrospective study, we enrolled consecutive patients with unilateral ICA or MCA occlusion confirmed by MRA, computed tomography angiography or Digital subtraction angiography (DSA) from June 2015 to June 2017. Patients with MCA and/or ICA stenosis were excluded. Patients with ipsilateral ICA ≥ 50% stenosis were excluded. Patents with evident cardioembolism and other pathologies such as vasculitis, dissection, and Moyamoya disease were excluded. Symptomatic patients were defined as having an ischemic stroke/TIA within 90 days and asymptomatic patients were defined as having no history of ischemic event. All patients had underwent routine head MRI, Vessel Encoded Arterial Spin Labeling (VE-ASL) (technique: pseudo-continuous labeling scheme, labeling duration=1500ms, post labeling delay=2000ms) and Dynamic susceptibility contrast (DSC) perfusion imaging. VE-ASL was used to evaluate collateral circulation and DSC was used to assess cerebral vasoreactivity by mean transit time (MTT) map according to a previous study.[1] The VE-ASL perfusion information was combined with 3-colored cerebral blood flow maps of the left carotid, right carotid, and posterior circulation territories. The presence of collateral flow was identified by the color compared with the standard anterior cerebral artery/MCA flow territory obtained from volunteers. Variants of Circle of Willis including missing A1 segment and fetal type posterior cerebral artery were carefully and thoroughly considered. The intensity of collateral flow was categorized as: Grade 1, collateral flow distributed less than 1/3 target downstream territory; Grade 2, collateral flow distributed within 1/3-2/3 target downstream territory; Grade 3, collateral flow distributed more than 2/3 target downstream territory. The pattern of collateral flow was categorized as: A. Anterior dominant pattern: collateral flow mainly originated from anterior cerebral artery(ACA) by anterior communicating artery or leptomeningeal collateral; B. Posterior dominant pattern: collateral flow mainly originated from posterior cerebral artery(PCA) by posterior communicating artery or leptomeningeal collateral; C. Anterior and posterior pattern: collateral flow equally originated from ACA and PCA. Relative MTT value, as well as other parameters, were calculated by volumetric measurements of affected territory divided normal territory. If patients also had underwent DSA, the DSA data were collected. Collateral pattern and intensity were graded by a scaling system named Collateral index score which represented the origination and robustness of collateral.[2] Comparison between asymptomatic group and symptomatic group was conducted using student’s t-test/Mann-Whitney test and Chi-squared test.Results
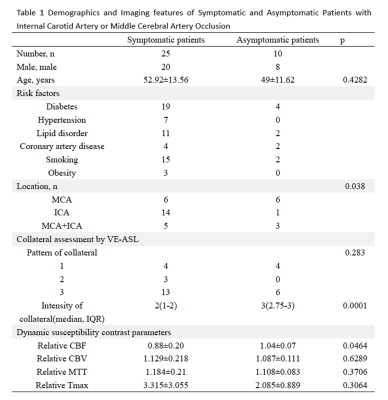
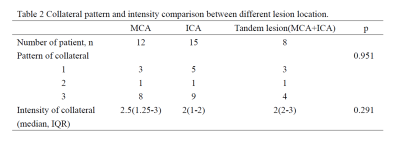
Totally, 35 patients (51.80±12.99 years, 28 men) including 25 symptomatic and 10 asymptomatic patients were recruited. Twelve patients had also underwent DSA. Kappa was 0.815 for the intensity of collateral and was 0.855 for the pattern of collateral between collateral evaluation by VE-ASL and DSA. In VE-ASL, The intensity of collateral in asymptomatic patients was significantly better than symptomatic patients (median 3, interquartile range(2.75-3) versus median 2, interquartile range(1-2), P=0.0001), whereas the pattern of collateral showed no significant differences (Table 1). Collateral intensity and pattern showed no significantly different between different lesion location (Table 2). In DSC, relative cerebral blood flow value was significantly greater in the asymptomatic group than the symptomatic group. Relative MTT value showed no significant differences. Risk factors were not significantly different between the symptomatic and asymptomatic group. Details please see Table 1. Figure 1 represents two typical cases with different collateral status.Conclusion
The present study indicates that hemodynamic impairments in symptomatic patients with ICA/MCA occlusion may be mainly induced by the insufficiency of collateral circulation. As a feasible and useful approach to evaluate the intensity and pattern of collateral flow, VE-ASL may be helpful in stratifying high-risk patients with ICA/MCA steno-occlusion.Acknowledgements
NoneReferences
1. Kawano T, Ohmori Y, Kaku Y, et al. Prolonged Mean Transit Time Detected by Dynamic Susceptibility Contrast Magnetic Resonance Imaging Predicts Cerebrovascular Reserve Impairment in Patients with Moyamoya Disease. Cerebrovascular Diseases, 2016: 131-138.
2. Alali F, Jefferson A, Barrow T, et al. The capillary index score: rethinking the acute ischemic stroke treatment algorithm. Results from the Borgess Medical Center Acute Ischemic Stroke Registry. Journal of NeuroInterventional Surgery, 2013, 5(2): 139-143.
Figures