4827
Unruptured Intracranial Aneurysms: Relationship between Wall Enhancement and Rupture Risk Factors Based on High-resolution Magnetic Resonance Imaging1Radiology, University of California, San Francisco, San Francisco, CA, United States, 2Radiology, Changhai Hospital, Shanghai, China
Synopsis
Wall enhancement (AWE) of intracranial aneurysms (IAs) on high-resolution black blood MRI has been described in ruptured aneurysms. This study investigated 103 unruptured saccular IAs and aims to assess the association between AWE and traditional risk factors and estimated one-year and five-year rupture risk estimated from previous large trails. We found aneurysms with AWE had more than 3 times higher estimated rupture risk (one-year and 5-year, 2.2% and 6.7%) than aneurysms without AWE (0.6% and 2.0%), and AWE was associated with traditional risk factors (size, location, symptoms). Identifying AWE may improve the risk assessment of IAs.
Introduction
Wall enhancement of intracranial aneurysms on high-resolution black blood magnetic resonance imaging (HR-MRI) has been described in ruptured aneurysms 1. Size, location and other risk factors are also associated with an increased risk of rupture 2. The prospective Unruptured Cerebral Aneurysm Study (UCAS) 2 trail provides a one-year rupture risk calculator based on the location and size of the aneurysm from 6697 patients, and PHASE meta-analysis provides a five-year risk based on 8328 patients 3. This study sought to ascertain whether AWE in UIAs is correlated with traditional risk factors and conventional aneurysm properties. An additional objective of the study was to determine the association between AWE and the estimated one-year and five-year aneurysm rupture risk based on existing large cohorts of UIAs.Methods
Study Population: 93 consecutive patients (33 male, mean age 57±10 years) with 103 confirmed unruptured saccular IAs were recruited from June 2014 to March 2017. All patients underwent 3T MRI and 3D rotational DSA. Pre- and post-contrast T1-weighted 2D/3D black-blood fast-spin-echo MRI (SPACE)4 was performed. Scanning parameter: TR/TE 700-1000ms/10ms; resolution: 0.4mm*0.4mm in-plane and 2mm slice thickness (2D) and 0.5mm isotropic (3D). Image analysis: The degree of aneurysm wall enhancement (AWE) was categorized into 3 grades: grade 0 indicates no AWE, grade 1 represents enhancement less than that of the pituitary infundibulum, and grade 2 represents enhancement equal to or greater than that of the pituitary infundibulum. The pattern of AWE was assessed as none, focal (a small region of wall enhancement), heterogeneous (incomplete wall enhancement) and complete enhancement. Aneurysm morphological parameters were measured on DSA, including size, maximum aneurysm height, aspect ratio (ratio of size to neck diameter, AR) and size ratio (ratio of maximum aneurysm height to average parent vessel diameter, SR). One-year rupture risk was calculated by the UCAS calculator, and five-year rupture risk was calculated using PHASE calculator (www.kockro.com/en/calculators). Multivariate logistic regression was used to study the factors independently associated with AWE. Spearman’s rank correlation analysis and chi-square test were performed to investigate the association between AWE and rupture risk, morphological features and patients’ demographical characters.Results
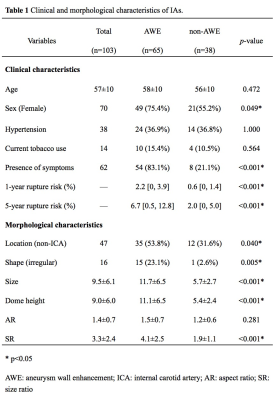
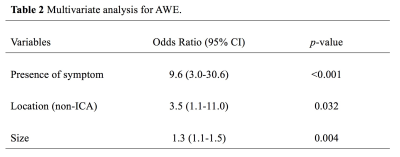
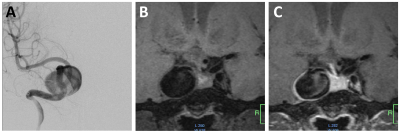
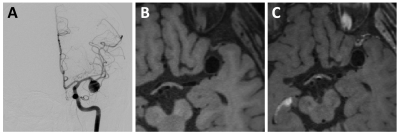
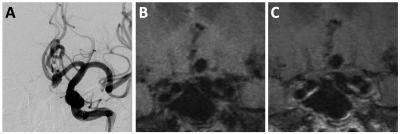
Patients demographics and aneurysm features with and without AWE are shown in Table 1. Aneurysms with AWE have more than 3 times higher estimated rupture risk (one-year and 5-year, 2.2% and 6.7%) than aneurysms without AWE (0.6% and 2.0%). Degree of AWE showed strong positive correlation with size (𝜌=0.60, p<0.001), maximum aneurysm height (𝜌=0.63, p<0.001) and SR (𝜌=0.62, p<0.001), and weak correlation with AR (𝜌=0.31, p=0.002). Larger area of AWE was strongly correlated with size (𝜌=0.64, p<0.001), maximum aneurysm height (𝜌=0.65, p<0.001) and SR (𝜌=0.63, p<0.001), and weakly correlated with AR (𝜌=0.35, p<0.001). Multivariate logistic regression analysis (Table 2) revealed that the presence of symptoms (OR 9.6, 95% CI 3.0-30.6, p<0.001), non-ICA location (OR 3.5, 95% CI 1.1-11.0, p=0.032) and size (OR 1.3, 95% CI 1.1-1.5, p=0.004) were independently associated with AWE. There’s no relationship between AWE and age, hypertension and current smoking. Sample images of patients with Grade 0-2 AWE are shown in Figure 1, 2 and 3.Discussion
To our knowledge, this is the current largest cohort study of unruptured intracranial aneurysm wall enhancement with more than 100 aneurysms, and this is also the first study to report the relationship between AWE and estimated short- and medium-term rupture risk. We found stronger and larger area of intracranial aneurysm wall enhancement were associated with its rupture risk and the traditional risk factors. This indicates that unruptured intracranial aneurysms with strong and large area of AWE maybe need to be monitored more frequently. The major limitation of current study is the lack of actual outcome (rupture or growth). Due to the low rupture rate in the intracranial aneurysm, much larger scale prospective studies with long follow-up duration are needed to clarify the role of wall enhancement in predicting intracranial aneurysm rupture.Conclusion
Prospective assessment of unruptured intracranial aneurysms wall enhancement with black blood MRI suggests that AWE associates with traditional risk factors and estimated short- and medium-time rupture risk. Identifying AWE may improve the risk assessment of UIAs.Acknowledgements
No acknowledgement found.References
1. Edjlali M, Gentric JC, Regent-Rodriguez C, Trystram D, Hassen WB, Lion S, et al. Does aneurysmal wall enhancement on vessel wall mri help to distinguish stable from unstable intracranial aneurysms? Stroke. 2014;45:3704-3706
2. Investigators UJ, Morita A, Kirino T, Hashi K, Aoki N, Fukuhara S, et al. The natural course of unruptured cerebral aneurysms in a japanese cohort. N Engl J Med. 2012;366:2474-2482
3. Greving JP, Wermer MJ, Brown RD, Jr., Morita A, Juvela S, Yonekura M, et al. Development of the phases score for prediction of risk of rupture of intracranial aneurysms: A pooled analysis of six prospective cohort studies. Lancet Neurol. 2014;13:59-66
4. Zhu C, Haraldsson H, Tian B, Meisel K, Ko N, Lawton M, et al. High resolution imaging of the intracranial vessel wall at 3 and 7 t using 3d fast spin echo mri. MAGMA. 2016;29:559-570
Figures