4808
Atherosclerotic Diseases in Entire Craniocervical Arteries and Aortic Arch and Stroke Risk: A 3D Multicontrast MR Vessel Wall Imaging StudyDongye Li1,2, Wei Dai3, Ying Cai4, Yongjun Han1, Guoen Yao3, Huijun Chen2, Chun Yuan5, and Xihai Zhao2
1Centre for Brain Disorders Research, Capital Medical University and Beijing Institute for Brain Disorders, Beijing, China, 2Center for Biomedical Imaging Research, Tsinghua University, Beijing, China, 3Department of neurology, The first affiliated hospital of the PLA general Hospital, Beijing, China, 4Department of Radiology, Taizhou People's Hospital, Taizhou, China, 5Department of Radiology, University of Washington, Seattle, WA, United States
Synopsis
Vulnerable atherosclerotic plaque in intracranial and extracranial carotid arteries and aortic arch is one of major causes of ischemic stroke. This study investigated the characteristics of atherosclerotic plaques in the craniocervical arteries and aortic arch and their relationships with stroke risk using 3D multicontrast MR vessel wall imaging. We found that high risk atherosclerotic plaques were most prevalent in intracranial arteries among three vascular beds. Combination of the maximum wall thickness in intracranial with extracranial carotid arteries might be a stronger predictor for cerebral acute ischemic lesions than that in each vascular bed alone.
Introduction and purpose
It has been shown that atherosclerotic disease in craniocervical arteries including intracranial and extracranial arteries and aortic arch is one of the major causes of ischemic stroke [1-3]. As such, accurate identification and characterization of atherosclerotic plaques in above vascular beds are important for patient management and stroke prevention. Currently, magnetic resonance (MR) vessel wall imaging has been demonstrated to be the most effective non-invasive approach in characterizing plaque features, particularly the utilization of the three-dimensional (3D) vessel wall imaging techniques with large coverage and isotropic high resolution [4-6]. However, the prevalence of atherosclerotic plaques in the craniocervical arteries and aortic arch in the same patient group and the predictive value of plaque burden in the entire craniocervical arteries and aortic arch for ischemic stroke remain unclear. The purpose of this study was to investigate the prevalence and characteristics of craniocervical arteries and aortic arch and their relationship with stroke risk using 3D multi-contrast MR vessel wall imaging.Methods
Study sample: Fifty-two patients (mean age, 56.3±13.4 years; 38 males) with recent cerebrovascular symptoms were enrolled and underwent multicontrast MR vessel wall imaging for craniocervical arteries and aortic arch. MR imaging: The MR imaging was performed on a 3.0T Philips MR scanner (Achieva TX, Best, The Netherlands) and custom-designed 36-channel coil with three imaging sections: intracranial artery: 3D T1-VISTA [4] and 3D SNAP [5]; extracranial carotid artery: 3D MERGE [6]and 3D SNAP; aortic arch: 3D PD-VISTA and 3D SNAP. The imaging parameters are detailed in Table 1. A routine protocol was performed for brain imaging by acquiring T1W, T2-FLAIR and DWI sequences. The study protocol was approved by institutional review board and written consent form was obtained from each subject. Image analysis: The MR images of intracranial and extracranial carotid arteries and aortic arch were reviewed separately by experienced radiologists. Presence/absence of atherosclerotic plaque and intraplaque hemorrahge (IPH) was determined at each vascular bed. The maximum wall thickness (Max WT) and luminal stenosis of each plaque were measured. Presence/absence of acute ischemic lesion (AIL) on DWI images was evaluated. Statistical analysis: The prevalence of plaques and IPH at each vascular bed was calculated. The correlation between atherosclerotic plaques in craniocervical arteries and aortic arch and AIL was determined using logistic regression and receiver-operating-characteristic curve (ROC).Results
Of 52 patients, 24 (46.2%) had AILs, and 30 (57.7%), 34 (65.4%), and 11 (21.2%) had plaques in intracranial artery, extracranial carotid artery, and aortic arch, respectively (Fig. 1). Intracranial arteries had the highest prevalence of IPH and severe stenosis (>50% stenosis), followed by extracranial carotid arteries and aortic arch (Fig. 1). Logistic regression analysis revealed that the Max WT in intracranial and extracranial carotid arteries but not in aortic arch was significantly associated with presence of AIL before and after adjusted for confounding factors (all p<0.05, Table 2). ROC analysis showed that, in predicting AIL, the Max WT of extracrannial carotid artery had the highest area-under-the-curve (AUC=0.72), followed by intracranial artery (AUC=0.70) and aortic arch (AUC=0.62). The AUC of Max WT of combined intracranial with extracranial carotid arteries reached 0.77 (Fig. 2, 3a-e).Discussion and Conclusion
In this study population, atherosclerosis and IPH were found to be most prevalent in intracranial and extracranial carotid arteries across entire craniocervical arteries and aortic arch. The maximum wall thickness of intracranial and extracranial carotid arteries was found to be independently associated with acute ischemic lesion. We found that the combination of the Max WT of extracranial artery with intracranial artery had stronger predictive value for acute ischemic lesion than each vascular bed alone.Acknowledgements
None.References
- Qureshi AI, Caplan LR. Intracranial atherosclerosis. The Lancet. 2014;383(9921):984-998.
- Gupta A, Baradaran H, Schweitzer AD, et al. Carotid plaque MRI and stroke risk: a systematic review and meta-analysis. Stroke. 2013;44(11):3071-3077.
- Di Tullio MR, Russo C, Jin Z, et al. Aortic arch plaques and risk of recurrent stroke and death. Circulation. 2009;119(17):2376-2382.
- Wang J, Helle M, Zhou Z, Bornert P, Hatsukami TS, Yuan C. Joint blood and cerebrospinal fluid suppression for intracranial vessel wall MRI. Magn Reson Med. 2016;75(2):831-838.
- Wang J, Bornert P, Zhao H, et al. Simultaneous noncontrast angiography and intraplaque hemorrhage (SNAP) imaging for carotid atherosclerotic disease evaluation. Magn Reson Med. 2013;69(2):337-345.
- Balu N, Yarnykh VL, Chu BC, Wang JN, Hatsukami T, Yuan C. Carotid Plaque Assessment Using Fast 3D Isotropic Resolution Black-Blood MRI. Magnetic Resonance in Medicine. 2011;65(3):627-637.
Figures
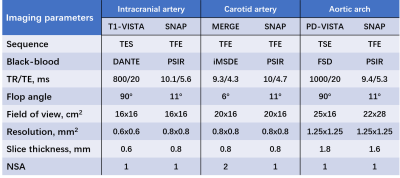
Table 1. The MR imaging protocol.
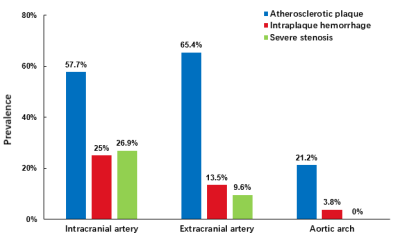
Figure 1. Prevalence of plaque
features in different vascular bed.
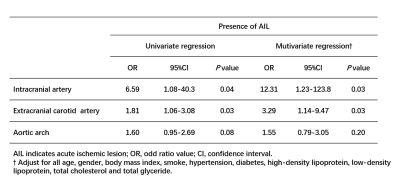
Table 2.
The correlation between atherosclerotic plaques in craniocervical
arteries and aortic arch and AIL by using logistic regression.
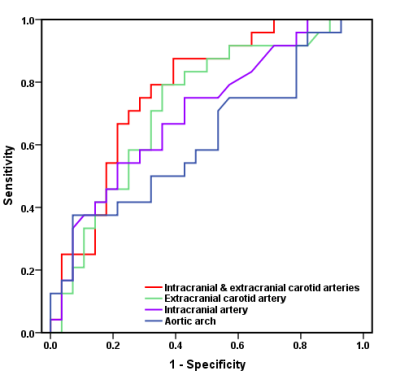
Figure 2. ROC curves
of Max WT of different vascular bed in discriminating AIL.
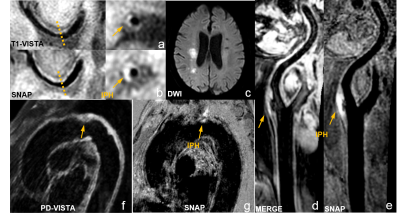
Figure 3. An
example for high risk plaques in intracranial (a-b, arrows) and extracranial carotid
arteries (d-e, arrows) with hyperintense IPH on SNAP images and AILs on DWI (c)
in the same patient. Example for high risk plaque with IPH in aortic arch of
another patient (f-g, arrows).