4777
Automatic Quantification of Left Ventricular Non-compaction using Fractal Dimension and Parametric Ratio as Geometric Markers: Numerical Simulation and Clinical Evaluation1Radiology, Texas Children's Hospital, Houston, TX, United States, 2Clements High School, Sugar Land, TX, United States, 3Cardiology, Texas Children's Hospital, Houston, TX, United States
Synopsis
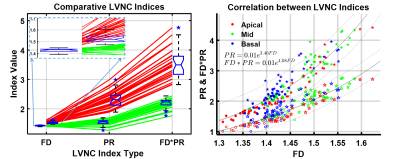
BSSFP distinguishes the non-compacted trabeculation (NC) from compacted myocardium (C), however the current diagnostic criterion (NC/C>2.3) for left ventricular non-compaction (LVNC) suffers from subjective variability and tends to over-diagnose, especially in pediatric patients where LV trabeculation varies on a continuous spectrum. Numerical simulations estimate exponential relationship between fractal dimension (FD) and perimetric ratio (PR) with 11 times higher dynamic range for PR for the observed FD range in 30 LVNC positive and 20 negative controls. Both FD and PR indices distinguish LVNC positive from negative (p<0.0001), while the PR and FD*PR provided 6 and 11 times higher dynamic ranges respectively.
PURPOSE
The purpose of this study is to investigate two-dimensional geometric markers viz. fractal dimension (FD) and perimetric ratio (PR) to quantitate irregularity and sparsity of the LV trabecular structures. Numerical simulations are used to evaluate the correlation and dynamic range of the PR compared to the previously reported FD [1]. We clinically evaluated the automatic quantification of LVNC in bright cine balanced steady-state free precession MR images using FD and PR in a pediatric cohort.BACKGROUND
Left ventricular noncompaction (LVNC) has possible major clinical manifestations such as congestive heart failure, arrhythmias and thromboembolism, including sudden cardiac death [2, 3], thus it is critical to identify these patients that require regular surveillance and likely activity restriction. Although MRI can reveal the non-compacted trabeculation (NC) distinctly from compacted myocardium (C), the current diagnostic criteria based on one dimensional measurements (NC/C>2.3) suffer from subjective variability and tend to over-diagnose left ventricular non-compaction (LVNC), especially in pediatric patients where LV trabeculation varies on a continuous spectrum [4].METHODS
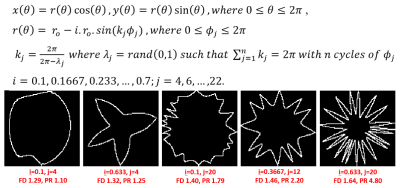
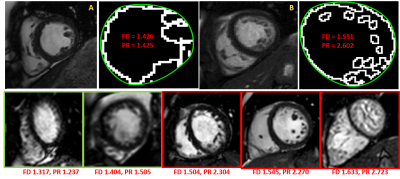
For the purpose of numerical simulations, the morphologic left ventricular endocardial boundary is represented in a binary image with a white circle of one pixel line width on a black background. In order to eliminate the influence of embedding space on FD calculation with the box counting method, square images centered at the circle and sides equal to the radius of the circle were created. The varying degrees of geometric irregularity of LV trabecular edge images is simulated using equations shown in Fig 1. Set of 10 simulated images were generated for each combination of amplitude (90% to 30% of original radius) and frequency (4 to 22 cycles over the entire perimeter) levels of variation in radius. The perimetric ratio (PR) is calculated as the ratio of the perimeter length of the spatially variant radius to the perimeter of the constant radius circle. Short-axis stack of end-diastolic bright blood MR images from 30 LVNC positive patients (age 15±5.0, range 4-30 yrs, 22 m; NC/C 2.8±0.38, range 2.3-3.6) and 20 LVNC negative patients (age 16±7.4, range 8-39 yrs, 11 m) were analyzed retrospectively using a novel automated tool. The only user interaction required was to select the most basal and apical slice to be included in the analysis. The tool automatically tracks the LV size and shape. Otsu’s thresholding algorithm delineates papillary and trabecular muscles. FD were computed on the resultant edge images using the box counting method. A piecewise closed Bézier curve of 2nd order geometric continuity was fitted through the salient points of the convex hull of these edges to obtain endocardial contours (Fig 2). The ratio of length of blood pool edges to endocardial contour perimeter (PR) was computed for each slice. Paired t-tests were performed between FD & PR and FD & FD*PR for all slices. Global LVNC index was calculated as the mean of the top half (MTH) of the slices sorted by particular index. Two sample t-tests were performed for FD, PR, and FD*PR between LVNC positive and negative patients.RESULTS
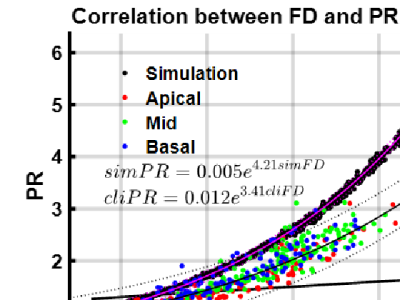
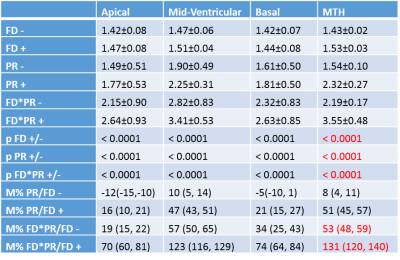
Numerical solutions generated 1000 binary trabecular edge images for a FD ranging from 1.26 to 1.69 with corresponding values of PR varying from 1.01 to 5.8. Representative simulated images are shown in Fig 1. Representative clinical images are shown in Fig2. The relationship between FD and PR for simulated images can be expressed as simPR = 0.005e 4.21simFD. The analysis was performed successfully in all subjects (149 apical, 165 mid-ventricular, and 136 basal slices) with a computation time of 5±2 sec per subject. Fig 3 shows an overlay of FD and PR values of the 136 basal, 165 mid-ventricular, and 149 apical slices from 50 clinical cases on simulation derived values. The relationship between FD and PR for simulated images can be expressed as cliPR = 0.005e 3.41cliFD. The mean±SD, p values and % change in median values with 95% confidence intervals are shown in Fig 4. Figure 5 shows a one to one line plot and box plots for all indices along with a scatter plot for all slices.CONCLUSION
In this study we described a novel tool as well as a novel index to automatically quantify LV trabecular irregularity and sparsity. Numerical simulations estimate relationship between FD and PR to be exponential with estimated dynamic range for PR 11 times higher than the calculated FD range in clinical data. Both FD and PR indices distinguish LVNC patients from negative controls, while the PR and FD*PR respectively provide 6 and 11 times higher dynamic ranges.Acknowledgements
No acknowledgement found.References
[1] Captur G, Muthurangu V, Cook C, Flett AS, Wilson R, Barison A, et al. Quantification of left ventricular trabeculae using fractal analysis. J Cardiovasc Magn Reson. 2013;15:36.
[2] Rigopoulos A, Rizos IK, Aggeli C, Kloufetos P, Papacharalampous X, Stefanadis C, et al. Isolated left ventricular noncompaction: an unclassified cardiomyopathy with severe prognosis in adults. Cardiology. 2002;98:25–32.
[3] Stöllberger C, Blazek G, Dobias C, Hanafin A, Wegner C, Finsterer J. Frequency of stroke and embolism in left ventricular hypertrabeculation/noncompaction. Am J Cardiol. 2011;108:1021–3.
[4] Petersen SE, Selvanayagam JB, Wiesmann F, Robson MD, Francis JM, Anderson RH, et al. Left ventricular non-compaction: insights from cardiovascular magnetic resonance imaging. J Am Coll Cardiol. 2005;46:101–5.
Figures