4755
Late gadolinium enhancement by cardiovascular magnetic resonance, combined with right ventricle ejection fraction, for assessing the severity and predicting the prognosis of chronic thromboembolic pulmonary hypertension1Radiology, Beijing Chaoyang Hospital, Beijing, China, 2Respiratory, Beijing Chaoyang Hospital, Beijing, China, 3Beijing Chaoyang Hospital, Beijing, China, 4Siemens Healthcare, Beijing, China
Synopsis
The aim of this study was to assess the severity and predict the prognosis of chronic thromboembolic pulmonary hypertension (CTEPH) using cardiovascular magnetic resonance with late gadolinium enhancement (LGE) combined with the right ventricle ejection fraction. Based on right heart catheterization, the percentages of the myocardial fibrosis volume (pFV>7.00%) and right ventricle ejection fraction (RVEF<34.34%) cut-off values were determined to assess the severity and predict the prognosis of 30 patients with CTEPH. The pFV and LGE are complementary to the RVEF for assessing the severity of the condition and can be a strong prognostic factor in patients with CTEPH.
Introduction:Pulmonary hypertension is a progressive disease of the pulmonary arteries, characterized by abnormally elevated pressure in the pulmonary circulation that results from extensive vascular proliferation and remodeling, progressing rapidly without treatment to right ventricular failure and death. In this disease, myocardial fibrosis in the interventricular insertion points is often seen, gradually leading to the involvement of the interventricular septum, likely due to increased right ventricle mechanical wall stress. The aim of this study was to assess the severity and predict the prognosis using late gadolinium enhancement (LGE) combined with the right ventricle ejection fraction in patients with CTEPH.
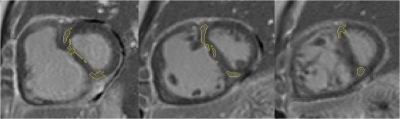
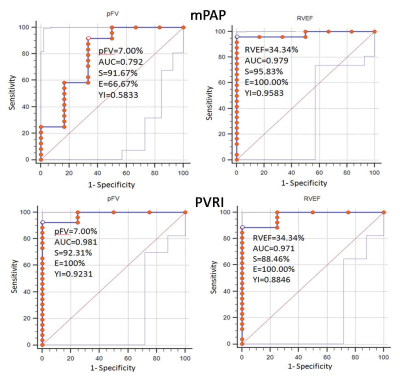
Methods: Thirty patients (age, 50.93±11.41 years, 50% males) with CTEPH were enrolled in our hospital from October 2013 to June 2017. The patients underwent LGE and cardiac function evaluation using cardiac magnetic resonance (CMR), with a detailed conventional evaluation including clinical history, right heart catheterization, and ultrasound. The CMR data were collected on a MAGNETOM Prisma 3T MR scanner (Siemens Healthcare, Erlangen, Germany) with an 18-channel body matrix receiver coil and a dedicated CMR protocol. Parameters of cardiac function, such as right ventricle ejection fraction (RVEF), were calculated on a workstation (cardiac analysis, Syngo Via MMWP VE30A, Siemens, Germany). Based on the mean pulmonary artery pressure (mPAP) and pulmonary vascular resistance index (PVRI) during right heart catheterization, the patients were divided into mild and moderate patients, and severe cases. The percentage of myocardial fibrosis volume (pFV) (Figure 1) and the parameters reflecting the right ventricle function were calculated. Receiver operating characteristic (ROC) curves were used for the data statistics to determine the cut-off values of the pFV to assess the severity of CTEPH. The patients were followed up from the first CMR examination to October 23, 2017. Death, lung transplantation, clinical symptom worsening, or hospitalization due to CTEPH was defined as end-point events. We attempted to analyze these characteristics and calculated the Kaplan-Meier survival curves in those patients who were treated using pulmonary endarterectomy (PEA) and anticoagulant therapy.
Results: Myocardial fibrosis was found in 29/30 (96.67%) of the CTEPH patients. The myocardial fibrosis volume (FV) in the PH patients was 8.39±6.14 ml, and the median pFV was 11.17%. Based on the mPAP and PVRI, the ROC curves (Figure 2) showed that pFV>7.00% and the right ventricular ejection fraction (RVEF)<34.34% was capable of distinguishing severe from mild and moderate CTEPH patients. In these 30 patients, eight underwent PEA, whereas 22 patients were treated with anticoagulant therapy. During the follow-up period of 16.1 months (median, 2.9-49), there were 20 patients with pFV>7.00% and RVEF<34.34%. Among these patients, two died within 30 days following PEA and the clinical symptoms of three patients in the anticoagulant therapy group worsened. We plan to expand the sample size to calculate the Kaplan-Meier survival curves and achieve more accurate results regarding prognosis.
Discussion& Conclusion: We determined the cut-off values of the pFV and RVEF in the ROC curves to assess the severity of CTEPH, factors that have a high sensitivity, specificity and accuracy. The mortality within 30 days after PEA and the probability of the occurrence of endpoint events in patients with CTEPH who had a pFV>7.00% combined with an RVEF<34.34%, were increased. This study showed that the LGE areas are complementary to the RVEF in the assessment of the severity of patients with CTEPH, and the investigation confirms and refines the evidence that LGE is a strong prognostic factor in patients with CTEPH, playing a complementary role with respect to RVEF.
Acknowledgements
No acknowledgement found.References
1. Freed B H, Gomberg-Maitland M, Chandra S, et al. Late gadolinium enhancement cardiovascular magnetic resonance predicts clinical worsening in patients with pulmonary hypertension[J]. Journal of Cardiovascular Magnetic Resonance, 2012, 14(1):1-9.
2. Bessa L G P, Junqueira F P, Bandeira M L D S, et al. Pulmonary Arterial Hypertension: Use of Delayed Contrast-EnhancedCardiovascular Magnetic Resonance in Risk Assessment[J]. Arquivos Brasileiros De Cardiologia, 2013, 101(4):336-343.
3. Oronzo C, Guido M, Mariarosa P, et al. Late gadolinium enhancement by cardiovascular magnetic resonance is complementary to left ventricle ejection fraction in predicting prognosis of patients with stable coronary artery disease[J]. J Cardiovasc Magn Reson, 2012, 14(1):1-8.
4. DiversC, Platt D, Wang E, et al. A Review of Clinical Trial Endpoints of Patients with Pulmonary Arterial Hypertension and Chronic Thromboembolic Pulmonary Hypertension and How They Relate to Patient Outcomes in the United States[J]. J Manag Care Spec Pharm, 2017, 23(1):92-104.
Figures