4749
Non-invasive MR-based blood oximetry via multi-parametric, non-linear estimation: initial multi-center experience in adult and pediatric patients1Dorothy M. Davis Heart and Lung Research Institute, The Ohio State University, Columbus, OH, United States, 2Northwestern University School of Medicine, Ann and Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States, 3Department of Biomedical Engineering, The Ohio State University, Columbus, OH, United States, 4Department of Electrical and Computer Engineering, The Ohio State University, Columbus, OH, United States, 5Cardiovascular MR R&D, Siemens Medical Solutions USA, Inc, Columbus, OH, United States, 6The Heart Center, Nationwide Children's Hospital, Columbus, OH, United States, 7Departments of Radiology and Biomedical Engineering, Northwestern University Feinberg School of Medicine, Chicago, IL, United States, 8Division of Cardiovascular Medicine, Department of Internal Medicine, The Ohio State University, Columbus, OH, United States, 9Department of Radiology, The Ohio State University, Columbus, OH, United States
Synopsis
Non-invasive estimation of blood oxygen (O2) saturation by magnetic resonance (MR) imaging would be useful in evaluating shunt severity in congenital heart disease, and oxygen delivery and consumption energetics in heart failure and pulmonary hypertension. A T2-based, non-linear, multi-parameter method has been developed to non-invasively determine O2 saturation in the heart and great vessels. In this multi-center study, the feasibility and accuracy of the technique is evaluated against gold-standard catheterization measurements in the cardiac chambers and vessels in a preliminary cohort of adult and pediatric patients with cardiovascular disease.
Introduction
Measurement of blood oxygen (O2) saturation levels in the right heart provides an index of systemic oxygen consumption, valuable in diagnosis and monitoring of patients with heart failure. O2 saturation also plays a role in shunt determination and interventional planning in patients with congenital heart disease (CHD). Invasive right-heart catheterization (RHC), which involves radiation exposure, is the current clinical standard to measure O2 saturation in the cardiac chambers and vessels. A T2-mapping-based, non-linear, multi-parameter estimation method was previously demonstrated to non-invasively determine blood O2 saturation in the heart1,2. In this multi-center study, the accuracy of the technique is evaluated against RHC in a preliminary cohort of adult and pediatric patients with cardiovascular disease.Methods
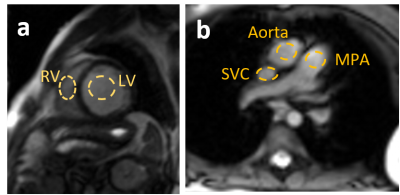
Thirty-seven patients (age, 42.0 ± 26.2 years; range, 22 months to 84 years; BMI, 25.8 ± 8.0 kg/m2; 15 females) undergoing clinically indicated RHC were recruited for the study across three centers. Twenty-four subjects (Center 1) were scanned on a 1.5T Magnetom Avanto system, nine subjects (Center 2) on a 3T Magnetom Skyra system, and four subjects (Center 3) on a 1.5T Magnetom Aera system (all Siemens Healthcare, Erlangen, Germany). For each patient, a series of T2-prepared single-shot steady-state free-precession (SSFP) images were acquired in free-breathing, across T2-preparation (T2p) times ranging from 0 to 200 ms. The corresponding inter-echo spacing (τ180) ranged from 0 to 25 ms. Images were acquired in a short-axis view of the right and left ventricles (RV and LV). Cross-sectional views of the superior vena cava (SVC), pulmonary artery (PA) and aorta were additionally acquired in a subset of 13 patients, leading to a total of 55 data sets available for analysis. The average acquisition time for each imaging plane ranged from 30 to 50 seconds. The signal was measured in each image in ROIs placed in arterial and venous blood (Figure 1); a reference measurement of arterial O2 saturation corresponding to a reference arterial blood pool (LV or the aorta), was obtained with a pulse oximeter (SpO2), and hematocrit was measured from a blood sample. These data were jointly processed to estimate the unknown venous O2 saturation and other remaining nuisance parameters of the Luz-Meiboom model (S0, T2O, τex, and α)3,4. O2 saturation of the RV, SVC or MPA were then compared to the corresponding catheterization results. In addition, six data sets (two from each center) were evaluated by two observers to establish reproducibility in data analysis across centers.Results
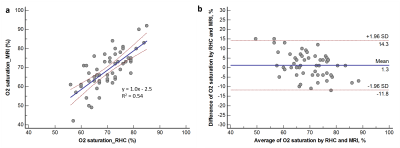
The average arterial SpO2 levels were 96 ± 4% (range, 76% to 100%), and average hematocrit levels were 39.5 ± 6.7% (range, 23.5% to 69.0%). The average heart rate at the time of imaging was 83 ± 17 bpm (range, 43 to 120 bpm). MRI and RHC measurements made within 24 hours were obtained for 35 patients, the remaining two patients had time differences of six and 28 days, respectively. Linear regression and Bland Altman plots comparing the MRI-derived estimates of O2 saturation against catheter measurements are shown for all data sets in Figure 2. A significant linear relationship was observed (y = 1.0x - 2.5%, p < 0.0001, R2 = 0.54). The average absolute mean difference between O2 saturation estimated by MRI and RHC was 5.5 ± 3.9% (range, 0% to 15%). Bland Altman analysis revealed a small, non-significant bias of 1.3% (p = 0.15) with limits of agreement ranging from -11.8% to 14.3%. The single-measures intra-class correlation coefficient was 0.97 (95% CI, 0.81 to 0.99), showing excellent agreement between observers.Discussion & Conclusion
The present study sought to evaluate the feasibility and accuracy of non-invasive MR oximetry in patients, across a wide age range and different presentations of cardiovascular disease such as heart failure, pulmonary hypertension, post heart transplant, and congenital heart defects (Tetralogy of Fallot, septal defects, Fontan etc). As shown by the significant linear relationship and small, non-significant bias, MR estimates of O2 saturation demonstrated a good agreement with the clinical standard O2 saturation RHC measurement. Larger differences between MR and RHC measurements of O2 saturation were generally observed in patients with known changes in hemodynamic state between the two exams. The result of this preliminary cohort of patients is encouraging, and indicates that the multi-parametric, non-linear approach to solve the L-M model may provide an effective strategy to non-invasively estimate O2 saturation, thus providing a useful tool for the diagnosis and monitoring of cardiovascular patients. Continuing studies aim at optimizing the image acquisition scheme and analysis, identifying suitable patient populations in whom the technique would be clinically beneficial, and addressing issues such as flow- and metallic-artifact-induced signal loss in the cardiac chambers and vessels.Acknowledgements
Funded by NIBIB R21EB021638, NHLBI 5T32HL098039-07 and TL1TR001423.References
1. Varghese J, Ahmad R, Jin N, Potter LC, Simonetti OP. Venous oxygen saturation estimation from multiple T2 maps with varying inter-echo spacing. J Cardiovasc Magn Reson. 2016;18(Suppl 1):W29.
2. Varghese J, Potter LC, LaFountain R, Pan X, Raman SV, Ahmad R, Simonetti OP. CMR-based blood oximetry via multi-parametric estimation using multiple T2 measurements. J Cardiovasc Magn Reson. 2017 (in press).
3. Wright GA, Hu BS, Macovski A. 1991 I.I. Rabi award. Estimating oxygen saturation of blood in vivo with MR imaging at 1.5 T. JMagn Reson Imaging. 1991;1(3):275–83.
4. Luz Z, Meiboom S. Nuclear magnetic resonance study of the Protolysis of Trimethylammonium ion in aqueous solution - order of the reaction with respect to solvent. J Chem Phys. 1963;39(2):366–70.
Figures