4742
GRASE Revisited: Breath-hold Three-dimensional (3D) Magnetic Resonance Cholangiopancreatography using a Gradient and Spin Echo (GRASE) Technique at 3T1Radiology, Seoul National University Hostpital, Seoul, Republic of Korea, 2Radiology, Seoul National University, Seoul, Republic of Korea, 3Seoul National University Hospital, Seoul, Republic of Korea, 4Seoul National University Hostpital, Seoul, Republic of Korea, 5Hallym University Sacred Heart Hospital, Gyeonggi-do, Republic of Korea, 6Philips MR Clinical Science, Best, Netherlands, 7Philips Healthcare Korea, Seoul, Republic of Korea
Synopsis
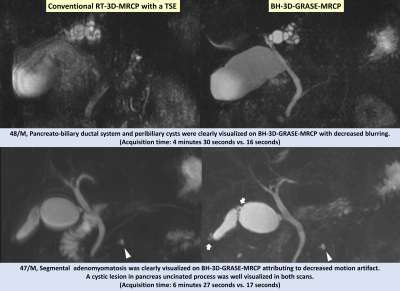
We evaluate the clinical feasibility and image quality of breath-hold (BH) three-dimensional (3D) MRCP using a gradient and spin-echo (GRASE) technique compared to the conventional 3D respiratory-triggered (RT)-MRCP using a turbo spin-echo (TSE) sequence at 3T. Sixty-six patients underwent both 3D RT-TSE-MRCP and 3D BH-GRASE-MRCP at 3T and three radiologists independently reviewed the images. The 3D BH-GRASE-MRCP had a significantly better image quality. In detail, 3D BH-GRASE-MRCP better depicted the common bile duct, cystic duct, and bilateral 1st intrahepatic duct. The number of scans with nondiagnostic or poor image quality significantly decreased with 3D BH-GRASE-MRCP compared with 3D RT-TSE-MRCP.
INTRODUCTION
Among various approaches to reduce scan time of MRCP, the 3D gradient and spin-echo (GRASE) technique1 had been previously proposed but have never actually taken hold as a standard protocol due to the failure to provide a consistent acceptable image quality compared with conventional 3D respiratory-triggered (RT) turbo spin-echo (TSE) MRCP. With the recent technological developments including the high SNR of 3T, a high fidelity gradient system, and improved field homogeneity, we can expect a better image quality from the GRASE MRCP.2 In this study, we further optimized the 3D GRASE sequence, because it can provide high speed and a relatively good SNR and is resistant to artifacts compared with other aforementioned sequences for BH-MRCP, which could exploit the advantages of this sequence at 3T. Therefore, the purpose of this study was to evaluate the clinical feasibility of the 3D BH-MRCP using 3D GRASE technique (BH-GRASE-MRCP) compared with conventional 3D RT-TSE-MRCP.METHODS
Sixty-six consecutive patients (mean age 58.6±14.1 years, M:F=34:32) underwent both conventional 3D RT-TSE-MRCP and 3D BH-GRASE-MRCP at 3T scanner sequentiallu, covering the same volume. Conventional MRCP was performed with TSE sequence. 3D BH-GRASE-MRCP was obtained using GRASE sequence1 and to reduce specific absorption rate and minimize TR, refocusing angle of 100º was applied after the initial 180º pulse. A combination of parallel acceleration factor and echo-planar imaging (EPI) factor was determined to minimize distortion. Following parameters were used: parallel acquisition factor, 2; turbo factor, 18; EPI factor, 7;and acquisition time, 9-18 seconds. Three abdominal radiologists independently reviewed the visualization of biliary and pancreatic ducts, image blurring, and overall image quality of the two datasets on four-point or five-point scales. The numbers of scans with nondiagnostic or poor image quality were compared between the two scans. The presence of biliary or pancreatic anatomic variation or disease were also evaluated.RESULTS
The mean acquisition time of the conventional 3D RT-TSE-MRCP were significantly longer than that of 3D BH-GRASE-MRCP (376.0±96.0 seconds [range: 255–788 seconds] vs. 15.6±1.4 seconds [9–18 seconds]; P<.0001). The 3D BH-GRASE-MRCP had a significantly better image quality (3.69±0.77 vs. 3.30±1.18, P=.005) and less image blurring (3.23±0.94 vs. 3.65±0.57, P=.0003) than that of the 3D RT-TSE-MRCP. The number of scans with the nondiagnostic/poor image quality decreased significantly compared with conventional 3D RT-TSE-MRCP (19.7% [13/66] vs. 1.5% [1/66], P=.002). Especially, 3D BH-GRASE-MRCP better depicted the common bile duct, cystic duct, and bilateral 1st intrahepatic duct (all Ps < .05), resulting in higher accuracy in diagnosing biliary anatomic variation (63.6-74.2% vs. 78.8-87.9%, statistically significant in one of the three readers; P=.04) and biliary diseases (statistically significant in one reader; P = .03). There were no significant differences in the diagnosis of pancreatic duct anatomy and pancreatic disease between the two MRCP datasets among all three readers (P=.27-1.0).DISCUSSION
The reduction in scan time and the better image quality of 3D BH-GRASE-MRCP can be explained by the advantages of the GRASE sequence. The GRASE sequence is a combination of the spin-echo and gradient-echo sequences, where several spin-echoes are replaced with gradient-echoes.1 This alteration between the RF refocusing pulse and the gradient within echo train allows improved temporal resolution compared with TSE sequence. Herein, we substantially accelerated the scan speed by adopting at turbo factor of 18, EPI factor of 7 and SENSE factor of 2. The reduced scan time may also explain the improved image quality of the 3D BH-GRASE-MRCP, as diaphragmatic up-down drift increasingly develops over time, decreasing the scan efficiency of the respiratory-triggered sequences.3 The better bile duct depiction and the improved overall image quality of the 3D BH-GRASE-MRCP led to a better diagnostic performance in some readers, unlike previous 3D BH-MRCP studies using non-CS techniques.1,4,5 Theoretically, GRASE is less prone to field inhomogeneity and chemical shift artifacts, because those effects evolve over a relatively short time compared to EPI.6 In addition, GRASE has no significant SNR loss despite the increased temporal resolution. As a spin-echo is used to fill the k-space center and a gradient-echo fills the periphery, giving a similar SNR to the SE sequence, the geometric distortion and signal loss can be reduced. Furthermore, the signal loss of peripheral k-space may not affect the image quality of MRCP because MRCP relies on a strong intrinsic contrast between a fluid and the background.CONCLUSION
3D MRCP was feasible in single breath-hold using a GRASE sequence, and 3D BH-GRASE-MRCP had a better image quality and reduced number of nondiagnostic images than that of conventional 3D RT-TSE-MRCP.Acknowledgements
No acknowledgement found.References
1. Wielopolski PA, Gaa J, Wielopolski DR, Oudkerk M. Breath-hold MR cholangiopancreatography with three-dimensional, segmented, echo-planar imaging and volume rendering. Radiology. 1999;210(1):247-252.
2. Martin DR, Friel HT, Danrad R, De Becker J, Hussain SM. Approach to abdominal imaging at 1.5 Tesla and optimization at 3 Tesla. Magnetic Resonance Imaging Clinics. 2005;13(2):241-254.
3. Taylor AM, Jhooti P, Wiesmann F, Keegan J, Firmin DN, Pennell DJ. MR navigator‐echo monitoring of temporal changes in diaphragm position: Implications for MR coronary angiography. Journal of Magnetic Resonance Imaging. 1997;7(4):629-636.
4. Morita S, Ueno E, Masukawa A, Suzuki K, Machida H, Fujimura M. Defining juxtapapillary diverticulum with 3D segmented trueFISP MRCP: comparison with conventional MRCP sequences with an oral negative contrast agent. Japanese journal of radiology. 2009;27(10):423-429.
5. Glockner JF, Saranathan M, Bayram E, Lee CU. Breath-held MR cholangiopancreatography (MRCP) using a 3D Dixon fat-water separated balanced steady state free precession sequence. Magn Reson Imaging. 2013;31(8):1263-1270.
6. Feinberg DA, Kiefer B, Johnson G. GRASE improves spatial resolution in single shot imaging. Magnetic resonance in medicine. 1995;33(4):529-533.