4711
Splenic MR Elastography in Prediction of Esophageal Varices Grading1Radiology, Chang-Hua Christian Hospital, Chang-Hua, Taiwan, 2Biomedical Imaging and Radiological Sciences, National Yang-Ming University, Taipei, Taiwan, 3Ministry of Health and Welfare, Taipei, Taiwan
Synopsis
To investigate the relationship between splenic MR elastography (MRE) and esophageal varices (EV). 167 patients underwent endoscopy and abdominal MR examination within 3-months interval were enrolled. MRE was performed with passive driver on right and left chest wall separately. The mean stiffness value of liver and spleen was determined. A good correlation between splenic stiffness and EV, but no correlation for liver stiffness was found. Our results demonstrated that spleen stiffness measured by MRE was significant correlated with EV grading. With 9.77 kPa spleen stiffness might be helpful in predicting presence of EV for patients with chronic liver disease.
Introduction
One of the major complications of portal hypertension is the development of esophageal varices (EV), which occur in approximately 30%–70% of patients with cirrhosis and have been shown to be correlated with the severity of liver disease. Screening endoscopy for EV is recommended for all patients with established cirrhosis. Unfortunately, endoscopy is invasive, uncomfortable, expensive, and time consuming and frequently requires sedation. Therefore, there is a clinical demand for a noninvasive method to assess esophageal varices. Magnetic resonance elastography (MRE) has been introduced as a noninvasive technology for the diagnosis and monitoring of liver stiffness. In addition, liver/spleen stiffness measured with MR elastography have been suggested as potential parameters to identify the presence of EV. The purpose of our study was to determine the utility of MR elastography in predicting the presence of esophageal varices in patients with liver cirrhosis.Materials and Methods
This retrospective study was approved and the informed consent was waived by our institutional review board. Finally, 167 patients (group 1, 69 patients without underlying liver disease; group 2, 37 with chronic liver disease but no liver cirrhosis; group 3, 61 with liver cirrhosis) underwent endoscopy and abdominal MR examination within 3-months interval were enrolled. All MRE images were obtained from a 1.5 Tesla scanner using a 16-channel phased array body coil. Two passive drivers were placed on patient’s right and left chest wall at the level of xiphoid simultaneously and imaging scan were performed separately. Continuous vibration waves of 60Hz were generated by active driver and the 2D gradient echo MR elastography was performed. A confidence map was created automatically. One radiologist who was blinded to patients’ clinical information performed the quantitative analyses of all images on workstation. The stiffness was calculated using the region of interesting (ROI) manually drawn on each elastogram with confidence mask. The ROI should be greater than 200 mm2 and avoid major blood vessels, obvious wave disturbance districts, and tumors. The mean stiffness value of liver and spleen was determined as follow: mean stiffness value =Σ stiffness value x ROI area/Σ ROI area. All endoscopic examinations were evaluated by one hepatologist who was blinded to the patients’ clinical information and MRE results. The grading of esophageal varices (EV) was according to modified Paquet classification (Grade I, Varices extending just above the mucosal level; Grade II, Varices projecting by one-third of the luminal diameter that cannot be compressed with air insufflation; Grade III, Varices projecting up to 50% of the luminal diameter and in contact with each other)Results
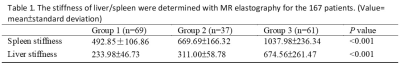
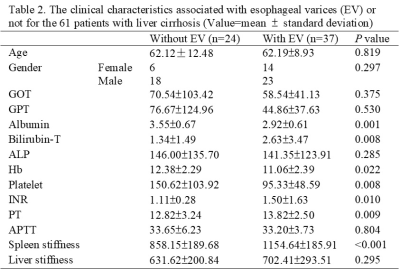
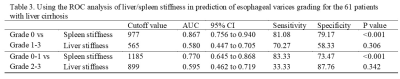
The liver and splenic stiffness values obtained when passive driver placed at right and left location are shown on Table 1. Significant correlation between mean liver and mean spleen stiffness values was observed among healthy liver and patients with varying degrees of chronic liver disease. Among patients with cirrhosis, the risk factors associated with esophageal varices were demonstrated on Table 2. The Albumin, bilirubin, hemoglobin, platelet, INR, prothrombin time and spleen stiffness showed significant difference between patients without EV and with EV. Liver stiffness showed no significant difference. Using the ROC analysis of liver/spleen stiffness in prediction of esophageal varices grading for the 61 patients with liver cirrhosis was shown on Table 3. The cutoff value was 9.77 kPa for differentiation of the group without EV from the group with EV of any grade and 11.85 kPa for differentiation of the group with grade I EV from the group with II/III EV.Discussions
The results of our study indicate that the spleen stiffness obtained with the passive driver placed on left chest wall was significantly correlated with healthy liver and patients with varying degrees of chronic liver disease. According to our results, spleen stiffness was useful in prediction of EV presence or not for patients with cirrhosis, but liver stiffness did not. With a cutoff value of spleen stiffness 9.77 kPa, 81% sensitivity and 79% specificity were demonstrated in differentiation of patients with EV from patients without EV.Conclusion
Our results demonstrated that spleen stiffness measured by MRE was significant correlated with esophageal varices grading. With 9.77 kPa spleen stiffness might be helpful in predicting presence of esophageal varices or not for patients with chronic liver disease. References:Acknowledgements
No acknowledgement found.References
1. Shin SU, Lee JM, Yu MH, et al. Prediction of esophageal varices in patients with cirrhosis: usefulness of three-dimensional MR elastography with echo-planar imaging technique. Radiology. 2014;272(1):143-53.
2.Talwalkar JA, Yin M, Venkatesh S, el al. Feasibility of in vivo MR elastographic splenic stiffness measurements in the assessment of portal hypertension. AJR Am J Roentgenol. 2009;193(1):122-7.