4697
Textural analysis of the morbidly adherent placenta (MAP) from MR acquisitions1Radiology, UT Southwestern Medical Center, Dallas, TX, United States, 2Department of Clinical Science, UT Southwestern Medical Center, Dallas, TX, United States, 3Advanced Imaging Research Center, UT Southwestern Medical Center, Dallas, TX, United States, 4Obstetrics & Gynecology, UT Southwestern Medical Center, Dallas, TX, United States
Synopsis
The morbidly adherent placenta (MAP) is a significant obstetric condition and hysterectomy is often the outcome for severe cases. We applied region of interest (ROI)-based texture analysis on retrospective placental MR images in women with history of placenta previa and previous cesarean deliveries. Our goal was to evaluate the textural characteristics of placental tissue in proximity to previous surgical scars and compare findings to surgical outcomes. Several significant Haralick texture features were seen in placental ROI’s near previous cesarean scars in those women who underwent hysterectomy.
Introduction
The morbidly adherent placenta (MAP) or placental invasion into the uterine myometrium in women with previous cesarean delivery has become increasingly prevalent, affecting 1 in 500 pregnancies1. Depending on the severity of placental invasion, patient management may involve a total hysterectomy at the time of cesarean delivery. The knowledge of morbidly adherent placenta severity prior to delivery allows for detailed operative planning to minimize the risk of uncontrolled bleeding at delivery. Although sonography is the recommended modality for diagnosing morbidly adherent placenta, MR imaging has been performed based on the hypothetical superior resolution and improved visualization of the entire placenta. We have recently applied textural analysis on placental ROIs from the standard grayscale clinical fetal MR images and showed textural-based correlations between placental heterogeneity and gestational age2. Currently, we sought to test this textural analysis for the prediction of hysterectomy at the time of cesarean delivery.Methods
With IRB approval, a retrospective review of 12 gravidas with ≥ 1 prior cesarean delivery who received an ultrasound and MR diagnosis of placenta previa or low-lying placenta in the third trimester (28-36 weeks) were obtained for feasibility purposes from our clinical database. All imaging data were acquired on a 1.5T MRI scanner (Avanto, Siemens Healthcare, Erlangen, Germany). The MR imaging studies included routine T2 weighted (T2W), T1 weighted (T1W), and diffusion-weighted (DW) imaging of the entire gravid uterus including the fetus and the placenta.
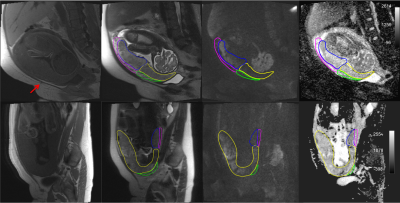
To investigate the texture feature difference between the invaded placental tissue/vasculature and the remaining placenta, we chose four regions of interest (ROIs) based on proximity to the cesarean scar (visible on T1W image). Imaging of ROIs from T2W, DWI (b=800 s/mm2), and ADC maps generated from the DWI series were evaluated. Specifically, two volumetric placental ROIs [in proximity to scar (abnormal ROI) and area remote from the scar (normal ROI)] and two volumetric placental vasculature ROIs (corresponding to the retroplacental areas) were identified in each placenta by an expert radiologist (Figure 1). All investigators were blinded to pregnancy outcome and MR reports.
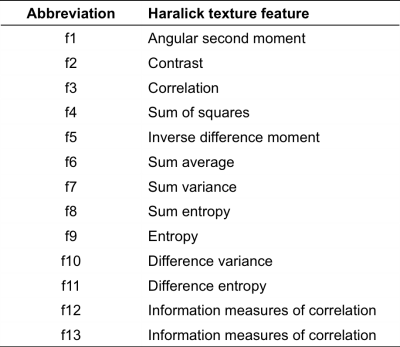
The 13 Haralick texture features (Table 1) with intensity normalization and histogram equalization were extracted using the Mahotas library and a custom written Python code for an OsiriX-based plugin. Differences between normal and abnormal ROIs were calculated on each slice for each textural feature respectively. A linear model was used to test the differences between hysterectomy and no hysterectomy cases with a random effect accounting for clusters of slices from the same patient. p value of less than 0.05 was considered statistically significant. The statistical analysis was performed using SAS software (Version 9.4, SAS Institute Inc., Cary, NC).
Results
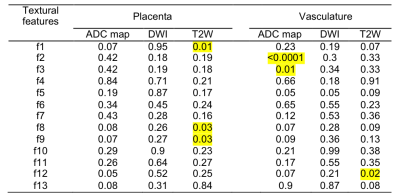
Of the 12 cases selected, 8 underwent cesarean hysterectomy and 4 had routine cesarean delivery. Table 2 shows the statistical difference based on textural features of placental ROI (normal vs. abnormal) and vasculature ROI (normal vs. abnormal). When comparing the hysterectomy and no-hysterectomy group, several textural features were identified to be statistically relevant. Figure 2 highlights distribution of the entropy textural metrics of placental ROIs in T2W image, where the abnormal placenta differed significantly from the normal placenta in the hysterectomy group (p<0.0001), but not in the no-hysterectomy group (p=0.9662). The contrast textural metric in vascularity ROIs on ADC maps was also significantly different between the normal vasculature and abnormal vasculature in both groups, but in the opposite direction.Discussion
We investigated the differences in textural features based on second order statistics on ROIs in areas in proximity to the cesarean scar artifacts seen on T1W to an area of the placenta remote from the scar(s) and the association with a high-risk surgical outcome. We demonstrated that there were statistically significant differences in textural features of the placenta when invasion was severe enough to result in cesarean hysterectomy. Textural mean values of the ROI’s between the hysterectomy and no-hysterectomy groups were also significantly different. We believe significant differences in contrast and entropy along with other textural features may be attributed to the architectural distortion of the cotyledons and abnormal villous vascularity of morbidly adherent placenta cases.Conclusion
Textural analysis of placental MR images may be helpful in characterizing individual patient risk for hysterectomy due to morbidly adherent placenta in women with previous cesarean delivery.Acknowledgements
No acknowledgement found.References
1. Rac MW, Dashe JS, Wells CE, Moschos E, McIntire DD, Twickler DM. Ultrasound predictors of placental invasion: the Placenta Accreta Index. Am J Obstet Gynecol 2015;212(3):343 e341-347.
2. Do QN, Lewis MA, Madhuranthakam AJ, Xi Y, Bailey A, Twickler DM. Application of texture analysis to apparent diffusion coefficient images of the normal human placenta. Proc Int Soc Mag Reson Med 2017;25:4822.
Figures