4695
Placental perfusion imaging using velocity-selective arterial spin labelingZungho Zun1,2,3,4 and Catherine Limperopoulos1,2,3,4
1Division of Diagnostic Imaging and Radiology, Children's National Medical Center, Washington, DC, United States, 2Division of Fetal and Transitional Medicine, Children’s National Medical Center, Washington, DC, United States, 3Department of Pediatrics, George Washington University, Washington, DC, United States, 4Department of Radiology, George Washington University, Washington, DC, United States
Synopsis
Recently placental perfusion imaging using velocity-selective arterial spin labeling (VSASL) was applied in pregnancies complicated by fetal heart disease. Here we demonstrate the feasibility of performing VSASL in the human placenta and provide supporting evidence that is needed for validation of placental VSASL. In our results, placental VSASL generated significantly higher ASL signal than pseudocontinuous ASL, showed high reproducibility, and demonstrated inflow-dependence. This study lays the groundwork for future investigation of placental perfusion imaging in pregnancies complicated by placental insufficiency.
INTRODUCTION
Reliable evaluation of in vivo placental function is important for detecting early deviation from normal fetal development, and is necessary to open a new, currently unavailable therapeutic window. Recently, placental perfusion imaging using velocity-selective arterial spin labeling (VSASL)1 was applied in pregnancies complicated by fetal heart disease, and revealed a significant difference in placental perfusion from healthy pregnancies2. In the current study, we demonstrate the feasibility of performing VSASL in the human placenta and provide supporting evidence that is needed for validation of placental VSASL.METHODS
Pulse Sequence: VS labeling was achieved with a cutoff velocity of 2 cm/s. Image acquisition was performed using fast-spin-echo 3D stack of spirals with 8 interleaves, TR/TE = 3000/10 ms, FOV = 36-40 cm, matrix size = 64x64, number of slices = 36-44, and slice thickness = 4 mm. Total scan time was 3:55 min. All scans were performed on a GE MR450 1.5 T scanner with an 8-channel cardiac coil. Comparison with pseudocontinuous ASL (PCASL): PCASL is the standard ASL method for measuring cerebral blood flow3. Placental VSASL and PCASL were performed in seven healthy pregnant volunteers (mean GA: 25±5 weeks) for comparison. PCASL was performed twice with two different labeling positions: 2.2 cm above and below the axial imaging slab. In PCASL, identical image acquisition to VSASL was used, labeling duration and post-labeling delay were 1450 ms and 2025 ms respectively, and total scan time was 4:10 min. Reproducibility: Placental VSASL scan was repeated back to back within the same scan session in fourteen healthy pregnant volunteers (mean GA: 28±5 weeks). Reproducibility was assessed using within-subject standard deviation (wsSD), within-subject coefficient of variation (wsCV), repeatability, and intraclass correlation coefficient (ICC)4,5. Response to Maternal Hyperoxia: Maternal hyperoxia was employed to modulate VSASL signal in the placenta by changing relaxation times of blood inflow in seven healthy pregnant women (mean GA: 30±6 weeks). 100% oxygen was inhaled through facial mask with rate of 15 L/min for 4-6 min. Varying Cutoff Velocity: As another way to modulate VSASL signal, cutoff velocity was varied from 2 cm/s to 4cm/s and infinity (i.e. no labeling) in six healthy pregnant women (mean GA: 32±2 weeks). Larger cutoff velocity was expected to generate the label farther from the imaging region, leading to reduced apparent VSASL signal.RESULTS AND DISCUSSION
Comparison with PCASL: Depending on the location of the placenta in the uterus, PCASL with one labeling location showed higher apparent placental perfusion than PCASL with the other labeling location. However, VSASL consistently showed substantially higher perfusion signal than PCASL using either labeling location (p < 0.01 for both; see Figure 1). Figure 2 shows comparison of VSASL and PCASL images acquired in two subjects. Reproducibility: Placental VSASL demonstrated high reproducibility based on the following parameters: wsSD = 7.1 ml/100 g/min (note that overall mean of placental perfusion in this experiment was 195 ml/100 g/min); wsCV = 3.5%; repeatability = 19.7 ml/100 g/min; ICC = 0.97. Figure 3 shows correlation and Bland-Altman plots of two repeated VSASL measurements. Response to Maternal Hyperoxia: Figure 4 compares the apparent placental perfusion with and without maternal hyperoixa as well as the results from the reproducibility test in the same subjects. The absolute difference (i.e. either increase or decrease) in placental perfusion between with and without hyperoxia was significantly larger than that of two repeated measurements without hyperoxia (p < 0.01). The inconsistent change of perfusion with hyperoxia may be because VSASL is sensitive to both T1 and T2 changes. Increased oxygenation with hyperoxia reduces T1 and increases T2 of blood, leading to reduction and increase in VSASL signal respectively. Overall VSASL signal change with hyperoxia may be positive or negative depending on actual changes of T1 and T2 in each subject. Varying Cutoff Velocity: Figure 5 shows the apparent placental perfusion measured using VSASL with cutoff velocity of 2 cm/s, 4 cm/s, and infinity. The differences between three measurements were all statistically significant (p < 0.01, for all).CONCLUSION
Placental VSASL generated significantly higher ASL signal than PCASL and showed high reproducibility within the same imaging session. Placenta VSASL was also found to be dependent on blood inflow based on modulation of VSASL signal using 100% oxygen inhalation and variation of cutoff velocity. This study supports the use of VSASL in placental perfusion imaging and lays the groundwork for future investigation of placental perfusion imaging in pregnancies complicated by placental insufficiency such as fetal growth restriction and preeclampsia.Acknowledgements
R01 HL116585-01 from NIH National Heart, Lung, and Blood Institute, and UL1TR000075/KL2TR000076 from the NIH National Center for Advancing Translational Sciences.References
1. Wong EC, Cronin M, Wu WC, et al. Velocity-Selective Arterial Spin Labeling. Magn Reson Med 2006;55:1334–1341. 2. Zun Z, Zaharchuk G, Niforatos-Andescavage N, et al. Non-invasive placental perfusion imaging in pregnancies complicated by fetal heart disease using velocity-selective arterial spin labeling. ISMRM 2017; Abstract 4806. 3. Dai W, Garcia D, de Bazelaire C, et al. Continuous flow-driven inversion for arterial spin labeling using pulsed radio frequency and gradient fields. Magn Reson Med 2008;60:1488–1497. 4. Bland JM, Altman DG. Measurement error. BMJ 1996;312:1654. 5. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull 1979;86:420–428.Figures

Figure 1. Apparent placental
perfusion measured using VSASL and PCASL with labeling planes above and below
the imaging slab. VSASL showed dramatically higher perfusion measurement than
either PCASL method in all subjects.
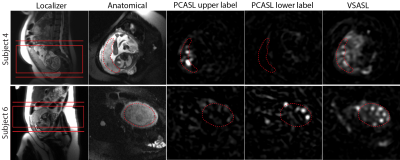
Figure 2. Comparison of placental
ASL images acquired using different labeling methods as well as localizer and
anatomical images in Subject 4 and 6 from Figure 1. The common imaging slab of
VSASL and PCASL and the two different locations of the labeling plane of PCASL
are shown in the localizer images. In the other images, the placenta is
delineated with the dotted line. For both subjects, VSASL signal in the
placenta was substantially higher than either PCASL scheme.

Figure 3. Correlation (a) and Bland-Altman (b) plots of
two repeated measurements of placental perfusion measured using VSASL back to
back in the same scan session. In b, solid and dotted lines represent the mean
difference and 95% limits of agreement respectively.

Figure 4. Apparent placental
perfusion in response to maternal hyperoxia compared to the repeated
measurements of placental perfusion before hyperoxia (baseline). With hyperoxia, apparent
placental perfusion decreased in Subject 1, 2, and 5, and increased in the
other subjects.
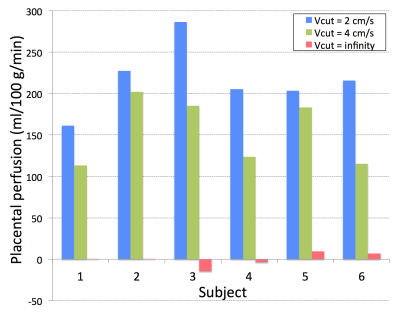
Figure 5. Apparent placental
perfusion measured using VSASL with cutoff velocity (Vcut) of 2 cm/s, 4 cm/s,
and infinity (i.e.no labeling). Apparent placental perfusion was reduced
significantly as cutoff velocity increased.