4684
Feasibility of Intravoxel Incoherent Motion (IVIM) Magnetic Resonance Imaging in Distinguishing Adenocarcinoma Originated from Uterine Corpus or Cervix1Department of Imaging Diagnosis, National Cancer Center/Cancer Hospital, Chinese Academy of Medical Science and Peking Union Medical College,Beijing,China, Beijing, China, 2GE Healthcare, China, Beijing, China
Synopsis
It is critical to distinguish adenocarcinoma arising from uterine corpus or cervix due to their different treatment methods and prognosis. However, it is hard to make a definite diagnosis based on MRI morphological characteristics, clinical examination., even the biopsy in some cases. The tumor biological information can be quantitatively evaluated by ADC and IVIM parameters(such as D, D* and f). Our study showed that ADC, D and f were significantly lower in the endometrial adenocarcinoma than the cervical adenocancinoma. IVIM parameters are promising biomarkers in predicting tumor origin of the uterine adenocarcinoma which contribute to treatment planning and prognosis evaluation.
Purpose
The aim of our study was to prospectively assess the possibility of the intravoxel incoherent motion (IVIM) MRI parameters in distinguishing the primary site of the adenocarcinoma.Methods
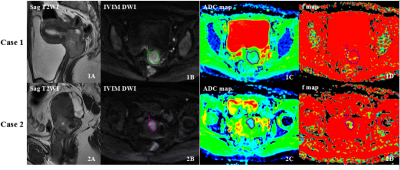
52 patients with consecutive uterine adenocarcinomas (median age, 53 years old; range, 25-74 years old) from the cervix (n=21) and endometrium (n=31) confirmed by surgery and pathology underwent IVIM MRI with 12 b value (0, 10, 25, 50, 75, 100, 150, 200, 400, 800, 1000, 1500, 2000 s/mm2.,NEX=2, 2, 2, 2, 2, 1, 1, 1, 1, 1, 4, 6, 6, respectively) examination before treatment at 3.0T MR scanner (GE Discovery 750, USA). Apparent diffusion coefficient(ADC)was calculated using monoexponential analysis(b=0,800 sec/mm2 ). A single representative region of interest (ROI) was manually drawn by one radiologist along the margin of the tumor on the IVIM DWI images of b1000, on the section containing the largest tumor cross-section area avoiding areas of necrosis and hemorrhage with reference to conventional MRI images T2WI and DCE MRI. All ROIs were directly co-localized on all parameter maps, then the software automatically generated the values of IVIM parameters and ADC(Figure1). ADC values and IVIM parameters including true diffusivity (D), perfussion-related diffusivity (D*) and perfusion fraction (f) were obtained from the FunctionTool mADC program (GE AW4.6, USA) and were compared by the two-sample t test and the Mann-Whitney U test. ROC was compared by MedCalc software and was used to evaluate the optiaml cut-off value and diagnostic efficiency of these parameters. P<0.05 was considered to indicate a statistically significant difference.Results
Results
Results
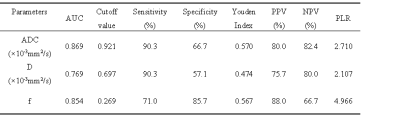
The ADC, D and f values were significantly lower in the endometrial adenocarcinoma than the cervical adenocancinoma (0.813×10-3mm2/s vs. 1.009×10-3mm2/s, 0.620×10-3mm2/s vs. 0.729×10-3mm2/s, 0.238 vs. 0.318, all the P value < 0.001), while no statistical difference of the D* existed between those two groups (P=0.271). Area under the curve (AUC) of ROC of ADC was higher than D (0.869 vs. 0.769, P=0.007) and f (0.869 vs. 0.854, P=0.759). Using the cut-off of ADC more than 0.921×10-3mm2/s to distinguish cervical adenocancinoma from endometrial adenocarcinoma, the sensitivity, specificity and accuracy were 90.3%, 66.7% and 80.8%, respectively(Table1).Discussion and conclusion
The cells of the endometrial adenocarcinoma are always arranged more compactly compared with that of cervical adenocarcinoma, which mostly present loosely tube- or branch-like arrangment, allowing larger intercelluar space and faster water molecular diffusion. And our results revealing lower diffusion parameters including ADC and D values in the endometrial adenocarcinoma were expected according to cell distribution described above. In addition, our results also showed the perfusion paremeter-f, related to the blood microcirculation, was siginificantly different between the two kinds of adenocarcinoma, which provide another perspective to determine the primary site of endometrial versus cervical tumors when the biopsy results are inconclusive. After all, it is not unusual for endometrial and cervical adenocarcinoma to share similar histologic charateristics like an endometrioid morphology and mucinous or squamous differentiation[1, 2]. The study indicated that IVIM MRI is a feasible technique to improve diagnostic performance in determining the origin of the uterine cancer.Acknowledgements
No acknowledgement found.References
[1] Bourgioti C, Chatoupis K, Panourgias E, et al. Endometrial vs. cervical cancer: development and pilot testing of a magnetic resonance imaging (MRI) scoring system for predicting tumor origin of uterine carcinomas of indeterminate histology[J]. Abdom Imaging. 2015, 40(7): 2529-2540.
[2] Vargas H A, Akin O, Zheng J, et al. The value of MR imaging when the site of uterine cancer origin is uncertain[J]. Radiology. 2011, 258(3): 785-792.