4680
Clinical feasibility of reduced field-of-view diffusion-weighted imaging for assessing the local extent of cervical cancer1Department of Radiology, Tokushima University, Tokushima, Japan, 2Department of Radiological Technology, Tokushima Bunri University, Sanuki-city, Japan
Synopsis
The diagnostic performance of reduced FOV DWI (rFOV-DWI) for assessing the local extent of surgically proven 24 cervical cancers was evaluated. The delineation of tumor margin on rFOV-DWI was assessed, and invasion to the vagina and parametrium evaluated on rFOV-DWI was compared with the histologically confirmed tumor extent. rFOV-DWI delineated the tumor margins better than T2WI and 3D DCE-MRI with statistically significance. Parametrial invasion and vaginal invasion as documented by rFOV-DWI agreed with the histopathological findings in 100% and 95% of cases, respectively.
Background and purpose of the study
Uterine cervical cancer is the 2nd or 3rd most common cancer in women, and caused by persistent infection with human papillomavirus. Treatment is stratified by clinical stage as delineated in the guidelines, and MRI is a potent tool to assess the tumor size and extension into the parametrium, vagina, or adjacent organs. DWI demonstrates cervical cancer as a high signal intensity mass, however, detailed evaluation of parametrial or vaginal invasion on conventional DWI is occasionally difficult due to low spatial resolution and distortion. Reduced phase direction field-of-view (FOV) technique by using spatially selective phase encoding gradient can offer high quality DWI with improved spatial resolution, without associated phase wrap round artifact, and with less artifacts related to motion and susceptibility which are common in larger FOV images 1-3). The purpose of this study is to compare the diagnostic performance of reduced FOV DWI (rFOV-DWI) with those of T2WI and 3D dynamic contrast-enhanced MRI (DCE-MRI) in evaluating local extent of cervical cancer.Materials and methods
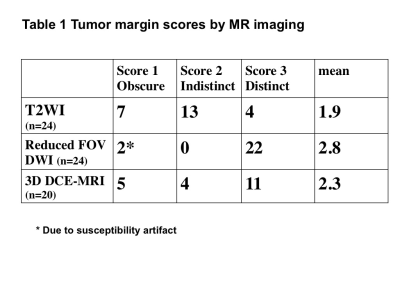
24 women with surgically proven cervical cancer (mean age, 47 years) who were undergone preoperative MRI including T2WI, and rFOV-DWI (FOCUS:FOV optimized and constrained undistorted single shot, FOV:20-24*10-12cm, Matrix:160*80, thickness:5mm, b = 50 and 800 sec/mm2) with/without 3D DCE-MRI (3D fast spoiled gradient-recalled echo sequence with fat-suppression; FOV:30cm, Matrix:320*192, thickness:3 mm/1.5 mm overlap; with intravenous administration of 0.1 mmol/kg of gadopentetate dimeglumine) with 3T MRI units (Discovery MR750, GE Healthcare) were included in the study. Tumor margins and tumor extent were evaluated on both sagittal and oblique axial (short axis) images with the consensus of two readers. Tumor margins were rated on a three-point scale as score 1: obscure, score 2: indistinct, and score 3: distinct. Evaluation of tumor extent included the presence of invasion to the vagina and parametrium, and the results were compared with the histologically confirmed tumor extent.Results and discussions
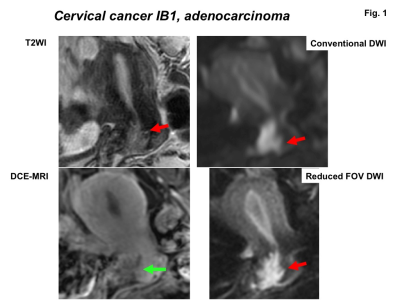
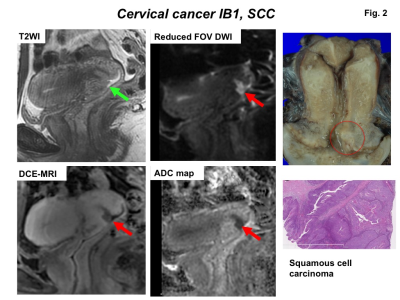
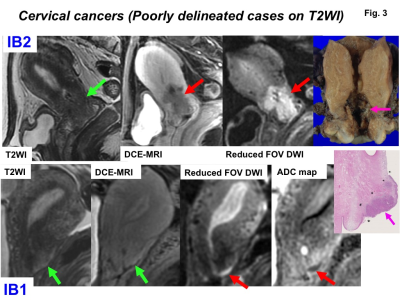
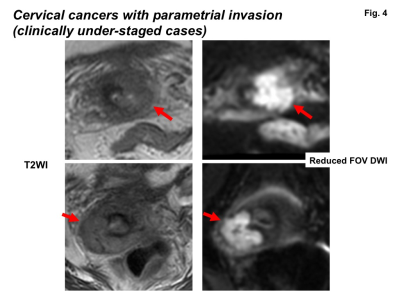
The 24 surgically proven cervical cancers included 3 FIGO stage IA, 14 IB1, 2 IB2, and 5 IIA1 tumors. Mean maximum tumor diameter measured on MRI was 24 mm (range 3-46 mm). The breakdown of the scores used to define the tumor margins by MR images is as follows: score 1 in 7 tumors, score 2 in 13 tumors, and score 3 in 4 tumors on T2WI; score 1 in 2 tumors (suboptimal due to severe susceptibility artifact), score 2 in 0 tumor, and score 3 in 22 tumors on rFOV-DWI; score 1 in 5 tumors, score 2 in 4 tumors, and score 3 in 11 tumors on DCE-MRI (Table 1). rFOV-DWI delineated the tumor margins better than T2WI and DCE-MRI (Fig. 1-3), with mean scores of 2.8, 1.9, and 2.3, respectively. The score of rFOV-DWI was statistically different from those of T2WI (P<0.001) and of DCE-MRI (P<0.05). rFOV-DWI could demonstrate even small lesions (≤20mm, n=10) as high intensity area with distinct tumor margin, whereas T2WI and DCE-MRI tended to show small lesions with obscure or indistinct margins. Histological examination revealed parametrial invasion in 2 cases (clinically under-staged), and each of three sequences could demonstrate parametrial invasion correctly in these cases (Fig. 4). On the other hands, each of three sequences overestimated vaginal invasion in 1 case, and T2WI underestimated vaginal invasion in 1 case but rFOV-DWI and DCE-MRI could demonstrate vaginal invasion in the case. Parametrial invasion and vaginal invasion as documented by rFOV-DWI (n=22, 2 suboptimal cases were excluded), T2WI (n=24), and DCE-MRI (n=20) agreed with the histopathological findings in all 22 patients (100%) and 21/22 patients (95%), all 24 patients (100%) and 22/24 patients (92%), and all 20 patients (100%) and 19/20 patients (95%), respectively.
According to the guidelines for the staging of cervical cancer with MRI, T2WI is essential, however, tumors sometimes did not well depicted on T2WI and the use of intravenous contrast medium or DWI may be recommended 4). Akita et al. reported the higher detectability of surgically proven cervical cancers on contrast-enhanced T1WI (95%) compared with that on T2WI (76%) 4). Park et al. reported high specificity (96-97%) and accuracy (90%) in assessing the parametrial invasion of cervical cancer on fused T2WI and DWI 5). In this study most lesions showed high intensity with distinct margins on rFOV-DWI except for 2 lesions with severe distortion caused by susceptibility artifact from adjacent rectal gas.
Conclusions
We conclude that rFOV-DWI may be useful for the detection and staging of cervical cancer in assessing the parametrial and vaginal invasion. rFOV-DWI can be an alternative to DCE-MRI in evaluating cervical cancer without the use of contrast medium.Acknowledgements
No acknowledgement found.References
1) Bhosale P, Ma J, Iyer R, et al. Feasibility of a reduced field-of-view diffusion-weighted (rFOV) sequence in assessment of myometrial invasion in patients with clinical FIGO stage I endometrial cancer. J Magn Reson Imaging 43:316-24, 2016.
2) Takeuchi M, Matsuzaki K, Harada M. Evaluating Myometrial Invasion in Endometrial Cancer: Comparison of Reduced Field-of-view Diffusion-weighted Imaging and Dynamic Contrast-enhanced MR Imaging. Magn Reson Med Sci 2017. [Epub ahead of print]
3) Ota T, Hori M, Onishi H,et al. Preoperative staging of endometrial cancer using reduced field-of-view diffusion-weighted imaging: a preliminary study. Eur Radiol 2017. [Epub ahead of print]
4) Akita A, Shinmoto H, Hayashi S, et al. Comparison of T2-weighted and contrast-enhanced T1-weighted MR imaging at 1.5 T for assessing the local extent of cervical carcinoma. Eur Radiol 21:1850-7, 2011.
5) Park JJ, Kim CK, Park SY, et al. Parametrial invasion in cervical cancer: fused T2-weighted imaging and high-b-value diffusion-weighted imaging with background body signal suppression at 3 T. Radiology 274: 734-41, 2015.
Figures