4644
3D Pseudocontinuous Arterial Spin-Labeling Perfusion Imaging Detected Crossed Cerebellar Daschisis at Acute, Subacute and Chronic Intracerebral Hemorrhage1Radiology, Peking University First Hospital, Beijing, China
Synopsis
Crossed cerebellar diaschisis (CCD) is the phenomenon of a decreased cerebellar perfusion and glucose metabolism in the cerebellar hemisphere contralateral to a supratentorial cerebral lesion. Although mostly seen in cerebral infarct, CCD has been reported in other clinical conditions such as intracerebral hemorrhage. Recently findings suggested that CCD is not just a neuroradiological phenomenon, arterial spin-labeling (ASL) is a novel noninvasive MRI method that uses arterial water as an endogenous tracer for perfusion imaging. The purpose of this study were to evaluate the value of 3D pCASL to detect CCD in different stage of ICH and to identify the relevant imaging or clinical factors of CCD development.
Introduction: Crossed cerebellar diaschisis (CCD) is not just a neuroradiological phenomenon, but an important prognostic indicator of stroke recovery and treatment response 1, 2. Few data on arterial spin-labeling based quantitative cerebral blood flow (CBF) in intracerebral hemorrhage (ICH) have been reported. The purpose of this study were to evaluate the value of 3D pseudocontinuous arterial spin-labeling (pCASL) perfusion imaging used to detect CCD in different stage of ICH and to identify the relevant imaging or clinical factors significantly associated with CCD.
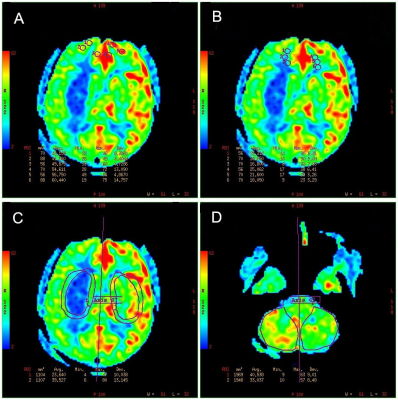
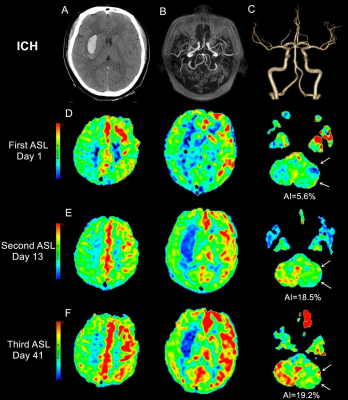
Methods: ASL perfusion images were prospective obtained from 16 patients with unilateral supratentorial ICH in acute, subacute and chronic stage. We assessed bilateral CBF values of different brain regions and the relationships between the CCD severity and other imaging findings, neurologic severity (NIHSS at admission and 14 days) and clinical outcome (mRS at 3 month).
Results: The ICH patients had significantly low CBF values of the contralateral cerebellum in acute, subacute and chronic stage. The hematoma volumes were significant positive correlated with the subacute and chronic CCD (r = 0.531, P = .034; r = 0.638, P = .008, respectively). The subacute CCD were significantly positive correlated with NIHSS score at 14 days (r = 0.614, P = .011) and mRS score at 3 month (r = 0.515, P = .041). The degree of supratentorial hypoperfusion in some regions were positively related to CCD severity.
Discussion: ASL could be used as a noninvasive alternative to SPECT for evaluating CCD3. In this study, we detected CCD in patients with unilateral supratentorial ICH at different stages. The subacute CCD were significantly correlated with clinical neurological defect (NIHSS score) and outcome (mRS score). The correlations means that, as the degree of cerebellar hypoperfusion in the subacute stage increases, the neurologic severity and clinical outcome worsens.
Conclusions: CCD in different stage of ICH can be detected by 3D pCASL perfusion imaging. With advantages in easy acquisition and noninvasive nature, 3D pCASL may be an ideal tool to study the phenomenon and clinical consequences of supratentorial hemorrhage with CCD.
Acknowledgements
No acknowledgement found.References
1. Seitz RJ, Azari NP, Knorr U, et al. The role of diaschisis in stroke recovery. Stroke 1999;30:1844-1850.
2. Szilagyi G, Vas A, Kerenyi L, et al. Correlation between crossed cerebellar diaschisis and clinical neurological scales. Acta Neurol Scand 2012;125:373-381.
3. Kang KM, Sohn CH, Kim BS, et al. Correlation of Asymmetry Indices Measured by Arterial Spin-Labeling MR Imaging and SPECT in Patients with Crossed Cerebellar Diaschisis. AJNR Am J Neuroradiol 2015;36:1662-1668.
Figures