4627
Magnetic resonance imaging features of parenchymal mass with tumor in vein in patients with cirrhosis1Liver Imaging Group, Radiology, San Diego, CA, United States, 2Dimagem Diagnostico por Imagem, Rio de Janeiro, Brazil
Synopsis
The purpose of this study is to determine in cirrhotic patients the proportion of MRI-diagnosed TIV cases with parenchymal masses, the proportion of cases due to HCC or non-HCC malignancy, and whether assessment of the parenchymal mass allows differentiation of the malignancy type. All TIV cases had parenchymal masses. Using a composite reference standard and excluding tumors with no reference standard, the underlying malignancy was HCC in 91% (41/45), ICC in 4% (2/45), and H-ChC in 4% (2/45). LI-RADS categorization of the parenchymal mass may help identify patients in whom TIV is not due to HCC. In particular, patients with TIV and LR-M parenchymal masses may need biopsy to exclude non-HCC malignancy.
INTRODUCTION
The Liver Imaging Reporting and Data System (LI-RADS) is an imaging-based diagnostic system applicable in patients at high risk of hepatocellular carcinoma (HCC). In LI-RADS, each liver observation is assigned a category that reflects probability of benignity, HCC, or other malignancy. In prior versions of LI-RADS, all tumors with tumor in vein (TIV) were categorized LR-5V, implying that all such tumors are HCC1. However, pathology studies indicate that both HCC and ICC can invade veins, with reported frequencies of 12-40% and 17-19% respectively2,3. Thus, assuming that all tumors with TIV are HCC is false. To reflect the fact that tumors other than HCC can invade veins, LI-RADS in 2017 renamed the category from LR-5V to LR-TIV4. Currently unknown are the proportion of LR-TIV cases associated with parenchymal masses, the proportion due to HCC or non-HCC, and whether imaging can reliably differentiate HCC vs. non-HCC causes of TIV. Therefore, the purpose of this study is to determine in cirrhotic patients the proportion of magnetic resonance imaging (MRI)-diagnosed TIV cases with parenchymal masses, the proportion of cases due to HCC or non-HCC malignancy, and whether assessment of the parenchymal mass allows differentiation of HCC vs non-HCC causes of TIV.METHODS
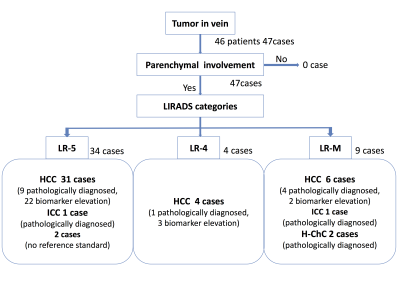
In this retrospective single-center study, the radiology information system was queried to identify 46 cirrhotic patients (35 men,12 women, aged 58.7 [30-80] years) with a total of 47 treatment-naïve malignant tumors with TIV diagnosed with MRI between 2009 and 2017. Two abdominal radiologists reviewed the MRI exams independently with subsequent consensus adjudication. The presence or absence of an associated parenchymal mass was determined. If a parenchymal mass was present, a LI-RADS v2017 category was assigned: LR-5 (Definitely HCC), LR-M (probably or definitely malignant, not specific for HCC), LR-4 (probably HCC). Histology and/or clinical biomarkers (AFP, AFP-L3, DCP, and CA19-9) were recorded if available (figure 1). The underlying malignancy was determined using a composite reference standard (all cases) and a histology reference standard (subset of cases with histology).RESULTS
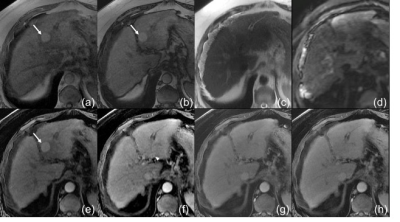
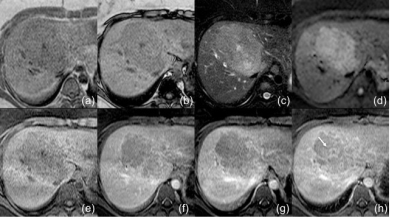
Parenchymal masses ranging in size from 3.5 to 25.6 cm (median 9.7 cm) were identified in all 47 cases and categorized retrospectively as LR-5 in 34 (74%), LR-M in 9 (19%), and LR-4 in 4 (9%). Of the 34 tumors with LR-5 masses, HCC was diagnosed in 31 (91%) based on pathology (n=9) or biomarker elevation (n=23), and intrahepatic-cholangiocarcinoma (ICC) in 1 (3%). In 2 of 34 tumors with LR-5 masses, no reference standard was available. Of the 9 tumors with LR-M masses, HCC was diagnosed in 6 based on pathology (n=4) or biomarker elevation (n=2), ICC was diagnosed in 1 based on pathology, and hepatocholangiocarcinoma (H-ChC) was diagnosed in 2 based on pathology. Of the 4 tumors with LR-4 masses, HCC was diagnosed pathologically in 1 and based on biomarker elevation in 3.DISCUSSION
In our limited series, all TIV cases had parenchymal masses. Using a composite reference standard and excluding the two tumors with no reference standard, the underlying malignancy was HCC in 91% (41/45), ICC in 4% (2/45), and H-ChC in 4% (2/45). Using a biopsy reference standard, the underlying malignancy was HCC in 78% (14/18), ICC in 11% (2/18), and H-ChC in 11% (2/18). The presence of parenchymal masses meeting LR-4 or LR-5 criteria predicted HCC as the etiology in 97% (35/36) or 91% (10/11), depending on whether a composite or biopsy reference standard was applied. Conversely, only 2/3 of TIV cases with LR-M masses were HCC; the others were ICC or H-ChC. Limitations of our study were its retrospective design, small sample size, and absence of histological proof in the majority of cases.CONCLUSION
While prospective confirmation is needed, ideally in a large multicenter study, our results suggest that virtually all cases of TIV have associated parenchymal masses detectable on imaging, that the large majority are due to HCC, and that LI-RADS categorization of the parenchymal mass may help identify patients in whom tumor in vein is not due to HCC. In particular, Patients with TIV and LR-M parenchymal masses may need biopsy to exclude non-HCC malignancy.Acknowledgements
We gratefully acknowledge the work of past and present members of Liver Imaging Group, Radiology, UC San Diego.References
1. American College of Radiology. CT/MR Liver Imaging Reporting and Data System version 2014. From http://www.acr.org/Quality-Safety/Resources/LIRADS.
2. Masami Minagawa, Treatment of hepatocellular carcinoma accompanied by portal vein tumor thrombus, World Journal of Gastroenterology,2006; 12(47): 7561-7567
3. Chong De Lu, Outcomes of intrahepatic cholangiocarcinoma with portal vein tumor thrombus following hepatic resection, Journal of Gastroenterology and Hepatology, 2016; 31(7): 1330-1335
4. American College of Radiology. CT/MR Liver Imaging Reporting and Data System version 2017. Nov. 2017, from http://www.acr.org/Quality-Safety/Resources/LIRADS.
Figures