4621
Comparison of Slice-specific Shim and Volume Shim for 1.5T Whole-body Diffusion Weighted Imaging1Guy's and St Thomas' Hospital, London, United Kingdom, 2MR Research Collaborations, Siemens Healthcare, Frimley, United Kingdom, 3MR Application Predevelopment, Siemens Healthcare, Erlangen, Germany, 4Division of Imaging Sciences, King's College London, London, United Kingdom
Synopsis
This study compared whole body diffusion weighted MR imaging (WB-DWI) acquired on a 1.5T scanner with and without integrated slice-specific shimming with retrospective distortion correction (iShim) for evaluation of monoclonal plasma cell disorders. WB-DWI with iShim showed significant reduction of the spinal displacement artefact and increased signal in the sternum.
Background
Whole-body diffusion weighted imaging (WB-DWI) is recognised as a sensitive and efficient technique for the evaluation of monoclonal plasma cell disorders1. However, distortion and signal reduction/voids remain as technical limitations of the technique, especially in regions of high susceptibility gradient. A prototype iShim sequence2 has been developed to reduce artefacts and distortion caused by B0 inhomogeneity by computing slice-specific centre frequency and linear shim terms, which are updated dynamically prior to each slice acquisition. Additionally, retrospective distortion correction is applied to correct for residual B0 inhomogeneities which are not corrected by linear shim terms2. A previous study investigating the use of iShim in WB-DWI studies showed a reduction in the negative impact of susceptibility effects at 3T3. The aim of this study is to confirm whether iShim also offers a significant improvement in image quality at 1.5T.Methods
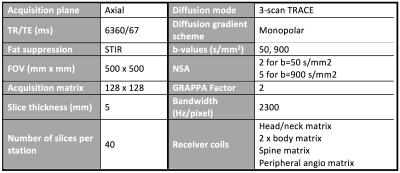
Following IRB approval and informed consent, 10 healthy volunteers (3 male, 7 female, median age 34 years, age range 24-38 years) were imaged on a 1.5T scanner (MAGNETOM Aera Siemens Healthcare, Erlangen, Germany). All volunteers underwent two WB-DWI examinations, one using the standard volume shim and one using iShim, in the same imaging session. The ‘Diffusion’ composing algorithm was selected for both sequences. Additionally, 24 sequential patients with evaluable WB-DWI examinations, scanned between April and October 2017, were identified from our database for inclusion in the study. 12 patients (7 male, 5 female, median age 80 years, age range 52-81 years) were scanned with the volume shim sequence and an independent group of 12 patients (4 male, 8 female, median age 59 years, age range 28-87 years) were scanned with the iShim sequence. The imaging sequences consisted of 7 contiguous stations from vertex to mid-calf. Acquisition parameters (Table 1) were identical for both sequences, excluding shimming method. Acquisition times were 23m 34s and 17m 51s for the iShim and volume shim sequences, respectively. The iShim acquisition time includes the time taken for field map acquisitions, required for frequency adjustment and shimming. The volume shim acquisition time does not include the time required for a 3D volume shim (approximately 30s per station).
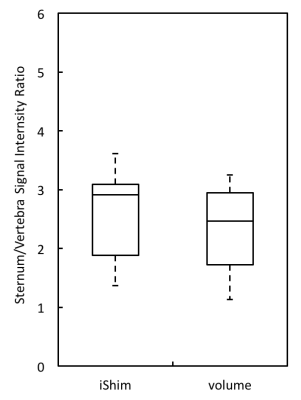
Images were analysed offline using the manufacturer’s post-processing software (Syngo.via, VB20A, Siemens Healthcare). All analysis was performed on sagittal thin MIPs reconstructed from axial b=900s/mm2 images. Presence/absence of spinal cord displacement artefact was recorded for all volunteer and patient scans at each junction between imaging stations 1-4. In each case the distance was measured from the anterior aspect of the spinal cord on the lower station to the anterior aspect of the spinal cord on the upper station. Volume shim and iShim patient studies were analysed independently by two experienced radiologists. Note was made of whether the presence of artefact could affect the interpretation of patient studies. Sternum-to-vertebra signal intensity ratios (SIRs) were calculated in order to assess signal loss in a region of high susceptibility gradient (sternum). 1cm2 circular regions of interest (ROIs) were drawn over the sternum and a relatively homogenous region (vertebral body), at the same vertical position, on a mid-sagittal slice of all volunteer scans. Sternum-to-vertebra SIRs were calculated from these measurements.
Results
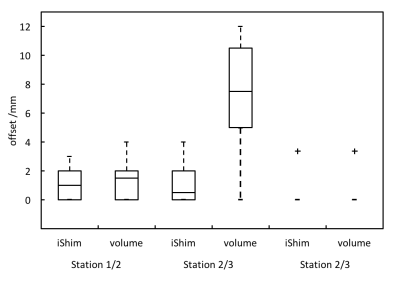
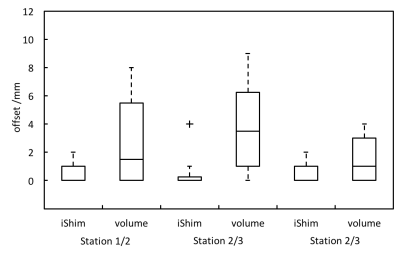
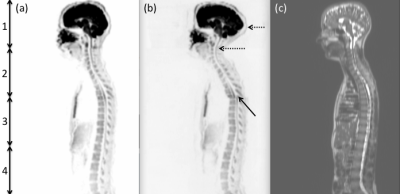
Figure 1 shows the distribution of spinal displacement artefact offsets in volunteers, which are significantly reduced at the junction of stations 2/3 using the iShim sequence (p<0.05, Wilcoxon rank sum test). This result is confirmed in patients, with significantly reduced mean offset at all junctions (Figure 2, p<0.05, Mann-Whitney U test). Figure 3 shows an exemplar case demonstrating the reduction of spinal displacement artefact at the junction of stations 2/3 on images of a healthy volunteer. Markedly reduced distortion in the head and cervical spine is also noted on the iShim image. The interpretation of the images could have been affected by the presence of artefacts in 2/12 patients and 0/12 patients scanned with the volume shim and iShim sequences, respectively. The sternum-to-vertebra SIR was significantly increased in the iShim images compared with matched volume shim images (Figure 4, p<0.02, paired t-test).Discussion
Slice-specific shimming and retrospective distortion correction resulted in a significant decrease in the ‘spinal-shift’ artefact and a significant increase in sternum-to-vertebra SIR in WB-DWI studies. Previous studies have shown that it is possible to reduce the spinal shift artefact by applying the centre frequency of one imaging station to all subsequent stations4; however, this method requires greater operator input and leads to a less streamlined workflow. Slice-specific shimming maintains a streamlined workflow, with only a small increase in imaging time. Importantly, iShim also reduced the likelihood of interpretation errors in patients related to artefact.Acknowledgements
No acknowledgement found.References
[1] C Messiou and M Kaiser, Br J Haematol. (2015) 171(1):29–37
[2] A Stemmer and B Kiefer Proc. Intl. Soc. Mag. Reson. Med. 23 (2015) #3729
[3] H Zhang, H Xue, S Alto, L Hui, S Kannengiesser, K Berthold and Z Jin, Invest Radiol (2016) 51:297-305
[4] D-M Koh, M Blackledge, AR Padhani, T Takahara, TC Kwee, MO Leach, DJ Collins. AJR Am J Roentgenol (2012) 199:252-262
Figures