4615
Late gadolinium MRI hyperintensity of colorectal liver metastases with extracellular contrast agents (gadobutrol) versus intravascular contrast agents (gadofosveset)1Department of Medical Imaging, Sunnybrook Health Sciences Centre, University of Toronto, Toronto, ON, Canada, 2Department of Surgery, Sunnybrook Health Sciences Centre, University of Toronto, Toronto, ON, Canada
Synopsis
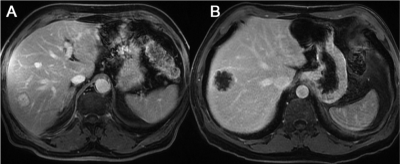
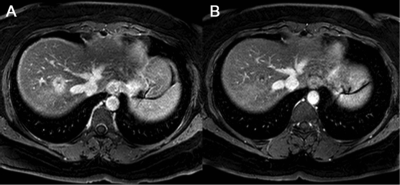
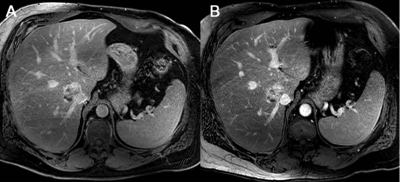
Late gadolinium hyperintensity (LGH) of colorectal liver metastases (CRCLM) using MRI with extracellular contrast agents presents a diagnostic dilemma that is commonly encountered clinically because it can be difficult to distinguish from benign hemangiomas. CRCLM may demonstrate less LGH using MRI with intravascular contrast agents due to reduced retention of contrast within these lesions. Approximately half of CRCLM demonstrate LGH on MRI with extracellular contrast agents versus only 6% on MRI with intravascular contrast agents. LGH is significantly better at excluding malignancy in patients with intravascular agents compared with extracellular contrast agents and may be a clinically useful problem-solving tool.
Introduction
Colorectal cancer is the second leading cause of cancer deaths in the developed world (1). Most deaths are related to metastatic disease, often to the liver. In recent years, surgery for colorectal liver metastases (CRCLM) has significantly improved morbidity and mortality and is now the standard of care (2). Preoperative imaging for detection and characterization of CRCLM (typically performed with MRI) is crucial for surgical planning (3). One of the signs used to characterize CRLM includes hypointensity on delayed phase MRI with extracellular contrast agents (4, 5). This sign is used because hemangiomas, the most common solid benign lesion in the liver, rarely demonstrate this sign. However, not all CRLM demonstrate this sign (6). CRLM that demonstrate hyperintensity on delayed phase MRI with extracellular contrast agents may be more difficult to diagnose given the overlap between benign and malignant findings. Unlike with MRI with extracellular contrast agents, CRLCM may not demonstrate retention of contrast with intravascular contrast agents (such as gadofosevest) based on several proof-of-concept studies (7-8).
Aim
The aims of this study were: (1) to determine the prevalence of CRLM that demonstrate late gadolinium hyperintensity (LGH) on MRI with extracellular contrast agent, gadobutrol, in a retrospective cohort, and (2) to determine the prevalence of LGH of CRLM on MRI with intravascular contrast agent, gadofosveset, compared to extracellular contrast agent, gadobutrol in a prospective cohort.Materials and Methods
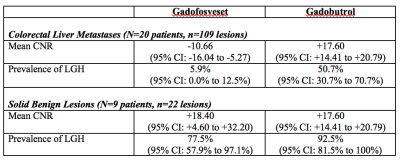
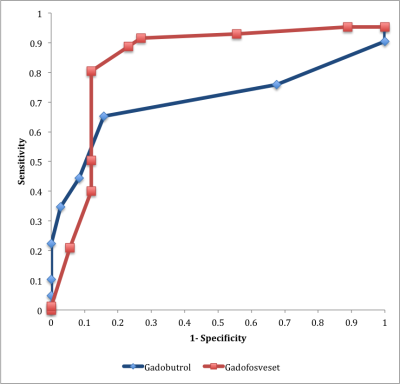
This study contains a retrospective and a prospective component, which were approved by the institutional research ethics board. In Part I, we determined the prevalence of pathology-confirmed CRLMs that demonstrate late gadolinium hyperintensity (LGH) on preoperative 10-minute delayed phase gadobutrol-enhanced MRI in a retrospective cohort of patients who received MRI between January 1, 2006 to December 31, 2012. In Part II, we performed a prospective study of patients with known colorectal cancer and suspected liver lesions who were referred for a contrast-enhanced liver MRI for diagnosis or staging. Patients received both a gadobutrol- and gadofosveset-enhanced MRI. The prevalence of LGH for all CRLMs and all solid benign lesions was determined at for both contrast agents. Receiver operating characteristics (ROC) curves were determined for contrast-to-noise ratio (CNR) as a predictor of malignancy for both contrast agents. The use of LGH to exclude malignancy using gadobutrol vs. gadofosveset was compared using the generalized estimating equation.Results
In Part I, there were 134 patients with 232 CRLMs who met inclusion/exclusion criteria. The prevalence of LGH of CRLMs on gadobutrol-enhanced MRI was 47.4% (95% CI: 39.5% to 55.4%). In Part II, there were 25 patients with 109 CRLMs and 22 benign solid lesions who met inclusion/exclusion criteria. The prevalence of LGH of CRLMs was 5.9% (95% CI: 0.0% to 12.5%) with gadofosveset versus 50.7% (95% CI: 30.7% to 70.7%) with gadobutrol. The prevalence of LGH of solid benign lesions was 77.5% (95% CI: 57.9% to 97.1%) with gadofosveset versus 92.5% (95% CI: 81.5% to 100%) with gadobutrol. The area under the ROC curve for CNR on 10-minute delayed phase MRI as a predictor of malignancy was 0.84 using gadofosveset versus 0.71 using gadobutrol. Both LGH (p=0.001) and the interaction of contrast agent and LGH (p=0.003) were statistically significant at excluding malignancy using the generalized estimating equation.Conclusion
Approximately half of CRLMs demonstrate LGH with gadobutrol, but few (approximately 6%) of CRLMs demonstrate LGH with gadofosveset. LGH with gadofosveset is better at excluding malignancy than LGH with gadobutrol. Gadofosveset-enhanced MRI may be a useful problem-solving tool in patients with colorectal cancer who have indeterminate focal liver lesions seen on conventional MRI.Acknowledgements
Thank you to Thayalasuthan Vivekanandan for administration support for this project.References
(1) Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A (2015). Global cancer statistics, 2012. CA Cancer J Clin 65:87-108
(2) Kanas GP, Taylor A, Primrose JN, Langeberg WJ, Kelsh MA, Mowat FS, et al. Survival after liver resection in metastatic colorectal cancer: review and meta-analysis of prognostic factors. Clin Epidemiol. 2012;4:283-301.
(3) Niekel MC, Bipat S, Stoker J. Diagnostic imaging of colorectal liver metastases with CT, MR imaging, FDG PET, and/or FDG PET/CT: a meta-analysis of prospective studies including patients who have not previously undergone treatment. Radiology. 2010;257(3):674-84.
(4) Low RN. Abdominal MRI advances in the detection of liver tumours and characterisation. Lancet Oncol. 2007;8(6):525-35.
(5) Garrett R. Solid liver masses: approach to management from the standpoint of a radiologist. Curr Gastroenterol Rep. 2013;15(12):359.
(6) Wilson SR, Kim TK, Jang HJ, Burns PN. Enhancement patterns of focal liver masses: discordance between contrast-enhanced sonography and contrast-enhanced CT and MRI. AJR Am J Roentgenol. 2007;189(1):W7-w12.
(7) Milot L, Haider M, Foster L, McGregor C, Law C. Gadofosveset trisodium in the investigation of focal liver lesions in noncirrhotic liver: Early experience. J Magn Reson Imaging. 2012;36(3):738-42.
(8) Cheung HM, Law C, Shoichet M, Karanicolas PJ, Coburn N, Milot L. Appearance of Focal Liver Lesions Using Contrast-Enhanced Magnetic Resonance Imaging Using Gadofosveset Trisodium, an Intravascular (Blood-Pool) Contrast Agent: A Pictorial Essay. Can Assoc Radiol J. 2016;67(3):242-9.
Figures