4605
Preoperative Prediction of Microvascular Invasion in Hepatocellular Carcinoma Using Radiomic Analysis of Diffusion-weighted MRI1MRI, the first affiliated hospital of zhengzhou university, zhengzhou,henan province, China
Synopsis
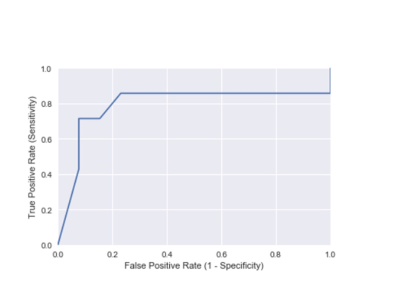
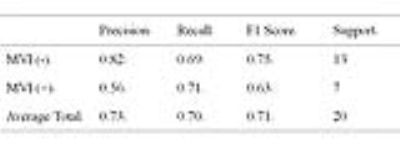
Microvascular invasion (MVI) in hepatocellular carcinoma (HCC) is an independent predictor of poor outcomes subsequent to surgical resection or liver transplantation (LT); however, MVI currently cannot be reliably determined preoperatively. In this study, we investigated the association between radiomic features on preoperative ADC maps and the MVI (with or without) in resected 96 HCCs. Furthermore, we employed machine-learning methods and independently evaluated their prediction performance. Total 1029 radiomic features were extracted from cancerous VOIs on ADC maps of each patient. Finally, 7 features could differentiate HCCs with MVI versus HCCs without. The random forest classifier using the optimal feature subset achieved the best performance, with an area under the receiver operating characteristic curve 0.79, sensitivity 71.0%, specificity 85.0%, precision 73%, and recall 70%.
Introduction
Microvascular invasion (MVI) in hepatocellular carcinoma (HCC) is an invasion of tumor cells into small vessels, which is an independent predictor of poor outcomes for patients undergone surgical resection or liver transplantation (LT). Unfortunately, MVI currently cannot be reliably determined preoperatively. Noninvasive clinical predictors and radiographic descriptors depending on subjective evaluation by individual radiologists have been proposed, however, the clinical impact of these biomarkers is unknown. It has been reported that ADC mean value can be a useful preoperative predictor of MVI(1), in addition, histogram analysis of ADC images show higher accuracy compared with that of ADC mean values, however, with a small sample size(2). In this study, we investigated the association between radiomic features on preoperative ADC maps and the MVI (with or without) in resected HCCs. Furthermore, we employed machine-learning methods and independently evaluated their prediction performance.
Purpose
To investigate the utility of DWI texture analysis to distinguish MVI-with HCCs from MVI-without, and propose a radiomics-based strategy for preoperative MVI prediction using texture features for HCC patients.Materials and Methods
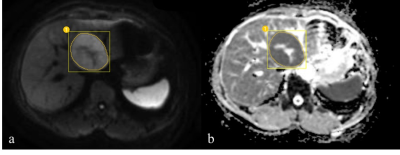
Patients who underwent resection of HCC from 2014 to 2017 were retrospectively analyzed. All patients included in the study had liver MRI within 1 month of surgery with a DWI protocol at a standard b value (b=0 and 800 sec/mm2) on a 3.0T MR scanner (Discovery MR 750; GE Medical Systems, Milwaukee, WI) with a torso coil (8CH HD Torso Array, GE Healthcare Coil). DW images were acquired using a single-shot echo-planar sequence in the axial plane; repetition/echo time, 3800/62 msec; slice thickness, 6mm; matrix, 256×256. Patients treated previously with ablation, embolization, resection or transplant or with gross macro-vascular invasion or with diffuse infiltrative pattern or with more than one HCC were excluded. In all, 96 patients with 96 HCCs (57 with MVI and 39 without MVI) were enrolled in this retrospective study according to their pathological results. We devided samples into two sets: the training set (n = 76 patients) and validation set (n = 20 patients). All DWI data was analyzed using in-house software written using MATLAB v. 7.6 (Mathworks, Natick, MA). All volumes of interest (VOIs) covering the entire tumor volume were delineated on DW images (b=800 sec/mm2) and the contours of VOIs were copied to corresponding ADC maps, as shown in Fig. 1. Total 1029 radiomic features were extracted from cancerous VOIs on ADC maps of each patient. These radiomic features quantify tumor phenotypic characteristics using tumor shape and size, intensity statistics, and texture. Variance threshold, selectKBest, and lasso regression model were used for data dimension reduction. The random forest(RF)classifier and logistic regression (LR) classifier were used with features selection and radiomics features building. The classification performance of the radiomics features was explored with respect to the receiver operating characteristics (ROC) curve.Results
The texture analyses on ADC maps showed that 7 features could differentiate HCCs with MVI versus HCCs without. Among 7 optimal features, two were texture features(Gray Level Co-occurrence Matrix and Gray Level Run Length Matrices), one were shape feature and four were intensity features. The top optimal discriminative feature was the Maximum3DDiameter of shape. The random forest classifier using the optimal feature subset achieved the best performance, with an area under the receiver operating characteristic curve 0.79, sensitivity 71.0%, specificity 85.0%, precision 73%, and recall 70%(Fig. 2 and Table 1).Discussion
Our findings showed that the histogram features and the Maximum3DDiameter were more correlated with MVI,which is consistent with previous finding (3). Meanwhile,We found that texture features of the ADC map also seem important for accurate prediction of HCCs with or without MVI. Theoretically, Gray Level Co-occurrence Matrix and Gray Level Run Length Matrices features can describe the complexity and heterogeneity of local intensity patterns, and potentially have discriminative power. Briefly, the novelty of this study is due to the use of radiomics features extracted from diffusion distributions, and the finding of an optimal feature set with favorable power on MVI prediction for HCC patients.Conclusion
Radiomic analysis from ADC maps can reflect the difference between with- and without-MVI HCCs. The proposed radiomics strategy using these features, combined with the random forest classifier, may better facilitate image-based MVI predicting for HCC patients preoperatively.Acknowledgements
No acknowledgement found.References
1.Xu P, Zeng M, Liu K, et al. Microvascular invasion in small hepatocellular carcinoma: is it predictable with preoperative diffusion-weighted imaging? J Gastroenterol Hepatol. 2014;29(2):330-336.
2. Huang YQ, Liang HY, Yang ZX, et al. Value of MR histogram analyses for prediction of microvascular invasion of hepatocellular carcinoma. Medicine. 2016;95(26):e4034. doi:10.1097/MD.0000000000004034.
3. Banerjee S, Wang DS, Kim HJ, et al. A computed tomography radiogenomic biomarker predicts microvascular invasion and clinical outcomes in hepatocellular carcinoma. Hepatology. 2015;62(3):792-800.
Figures