4592
Value of endovaginal MRI derived tumor volumes for predicting outcomes in patients selected for trachelectomy vs hysterectomy in cervical cancer1Institute of Cancer Research, Sutton, United Kingdom, 2The Royal Marsden NHS Foundation Trust, London, United Kingdom
Synopsis
A pre-surgical endovaginal MRI was performed in 142 women with early stage cervical cancer scheduled for hysterectomy (n=43) or trachelectomy (n=99). Total tumor volume was calculated by summing MRI and LLETZ/biopsy (done prior to imaging) volumes. In the hysterectomy group, tumour volume, grade and lymphovascular space invasion (LVSI) differed significantly between those without and with an adverse outcome (need for adjuvant treatment or recurrence); only volume and LVSI were significant in the trachelectomy group where multivariate analysis demonstrated their independence. In patients eligible for trachelectomy, with tumors >1.4 cm3 and with LVSI, administration of (neo)adjuvant treatment may potentially improve outcome.
Background
Early diagnosis of cervical cancer in young nulliparous women is driving an increasing demand for fertility-sparing procedures such as trachelectomy. Endovaginal MRI has increased sensitivity for detecting small volume tumors[1], [2] and is superior to conventional external array imaging[2]. However, the utility of defining volume of residual tumor on endovaginal MRI in addition to histological features of the tumor to predict subsequent outcome in patients selected for trachelectomy rather than hysterectomy has not been demonstrated.Aim
To establish whether total pre-surgical tumor volume in addition to histology was predictive of an adverse outcome in patients with small volume tumors selected for trachelectomy. Findings were compared to the significance of volume in larger tumors in patients selected for hysterectomy.Methods
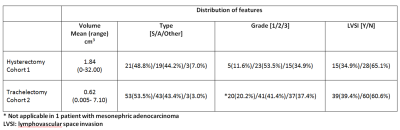
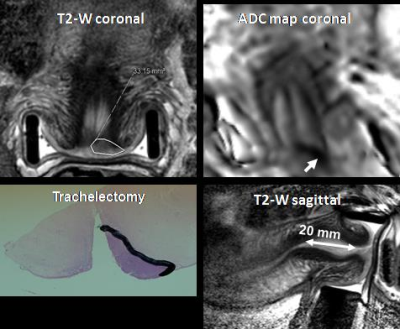
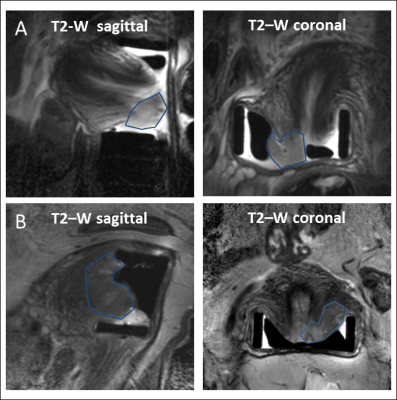
142 patients aged 23-63 years referred for endovaginal MR imaging were included. All had T2-W imaging in 3 planes orthogonal to the cervix (TR/TE 2750/80 ms (coronal and axial) and 2500/80 ms (sagittal); field of view (FOV) 100 mm x 100 mm; acquired (acq) voxel size 0.42 x 0.42 x 2 mm; reconstructed (recon) voxel size 0.35 x 0.35 x 2 mm; slice thickness 2 mm; slice gap 0.1 mm; 24 coronal and 22 sagittal slices; number of averages (NSA) 2) with matched Zonal Oblique Multislice (ZOOM diffusion-weighted imaging: TR/TE 6500/54; b-values 0, 100, 300, 500 , 800 s/mm2; FOV 100 x 100 mm; acq voxel size 1.25 x 1.25 x 2 mm; recon voxel size 0.45 x 0.45 x 2 mm; slice thickness 2 mm, slice gap 0.1 mm; 24 slices, NSA 1). MRI-derived tumor volumes were obtained by summing areas of ROIs that were manually segmented around tumor on T2W images and multiplying by slice thickness; ROIs were drawn with reference to information from diffusion-weighted scans for tumor identification. Total pre-surgical tumor volumes were calculated by summing endovaginal MRI derived volumes with volume of disease on a cone biopsy or LLETZ specimen obtained prior to imaging. Forty-three patients underwent subsequent hysterectomy (Cohort 1) and 99 underwent trachelectomy (Cohort 2). Univariate analyses (Mann-Whitney-U and Chi Squared test) were used to compare total volume, tumor type, grade and lymphovascular space invasion (LVSI) in those without and with an adverse outcome (defined as tumor recurrence or the need of adjuvant chemoradiotherapy due to adverse histology e.g. parametrial invasion [n=5], lymph node micrometastases [n=5], close or involved margins [n=9]). Receiver Operating Characteristic (ROC) curves were used to determine cut-off volumes for predicting adverse outcome. Multivariate analysis with Cox hazard ratio calculation (HR) was performed in Cohort 2, but not in Cohort 1 given the small number of patients with an adverse outcome in this group.Results
Tumor volumes and distribution of imaging and pathological features are given in Table 1. Twelve (27.9%) patients in Cohort 1 had an adverse outcome; 7 received adjuvant treatment, 3 had recurrent disease and 2 developed disease recurrence after adjuvant treatment. Adverse outcome was seen in 19 patients (19.2%) in Cohort 2; adjuvant treatment was given to 10 patients, 1 patient underwent subsequent hysterectomy, 8 demonstrated disease recurrence (including 1 after adjuvant treatment). In Cohort 1, total tumor volume (p=0.003), tumor grade (p=0.03) and LVSI (p=0.03) were predictive of adverse outcome. A cut-off volume of 1.84 cm3 indicated an adverse outcome with 85.7% sensitivity and 69.0% specificity. In the trachelectomy cohort, univariate analysis showed a significant result total tumor volume (p=0.04) and for LVSI (p=0.001). Multivariate analysis performed for these 2 features showed that total tumor volume (p=0.04; HR 1.4; [95% CI: 1.1-2.0]) and LVSI (p=0.001; HR 6.8; [95% CI: 2.1-22.3) were independent prognostic factors. A cut-off volume of 1.35 cm3 predicted adverse outcome with 52.6% sensitivity and 77.5% specificity (Fig. 2). At 80.0% specificity, total tumor volume had 64.3% sensitivity in the hysterectomy cohort and 31.6% sensitivity in the trachelectomy cohort for predicting adverse outcome.Conclusion
In patients selected for hysterectomy, where median tumor volumes were 1.84 cm3, tumor volume was an important factor when considering adverse outcome. For smaller tumors selected for trachelectomy, both volume and LVSI were predictive of outcome and independent, although the latter was more highly significant. Tumors >1.4 cm3 with LVSI being considered for trachelectomy may benefit from the routine use of neoadjuvant or adjuvant chemotherapy.Acknowledgements
CRUK and EPSRC support to the Cancer Imaging Centre at ICR and RMH in association with MRC and Department of Health C1060/A10334, C1060/A16464 and NHS funding to the NIHR Biomedical Research Centre and the Clinical Research Facility in Imaging.References
[1] N. M. deSouza, et al., “Cervical cancer: Value of an endovaginal coil magnetic resonance imaging technique in detecting small volume disease and assessing parametrial extension,” Gynecol. Oncol., vol. 102, no. 1, pp. 80–85, Jul. 2006.
[2] K. Downey, et al., “Comparison of optimised endovaginal vs external array coil T2-weighted and diffusion-weighted imaging techniques for detecting suspected early stage (IA/IB1) uterine cervical cancer-weighted imaging EPI Echo-planar imaging FIGO Federation Internationale Gynecology and Obstetrics FSE Fast spin-echo LLETZ Large loop excision of the transformation zone MRI Magnetic resonance imaging SENSE Sensory encoding SNR Signal-to-noise ratio TSE Turbo spin-echo,” Eur Radiol, vol. 26, pp. 941–950, 2016.
Figures