4568
An MRI assessment of inferior vena cava vessel morphology and venous flow in chronic hypertensive and normotensive pregnant women in the supine position.1Department of Perinatal Imaging and Health, Kings College London, London, United Kingdom, 2Perinatal Imaging and Health, Kings College London, London, United Kingdom, 3Faculty of Life Sciences and Medicine, Kings College London, London, United Kingdom, 4Department of Womens Health, Kings College London, London, United Kingdom
Synopsis
The supine position in pregnancy may develop supine hypertensive syndrome (SHS) caused by the gravid uterus compressing the inferior vena cava (IVC) and compromising venous return. The effect of positioning on vessel morphology and venous return in chronic hypertensive pregnant women has not been assessed. We used phase contrast imaging to assess matched groups of chronic hypertensive and normotensive women in the supine position. There were no significant differences in IVC morphology or venous return between the two groups, supporting the conclusion that chronic hypertensive women are not at higher risk than normotensives when supine.
Introduction
Pregnant women who lie supine may develop ‘supine hypotensive syndrome’ (SHS) secondary to inferior vena cava (IVC) compression by the gravid uterus. The reported incidences of SHS in normotensive pregnant women vary from none(1) to between 4% and 10%(2,3). The effect of the supine position in clinical cohorts such as chronic hypertensive pregnant women, who may be more vulnerable to blood pressure changes, has not been assessed. Chronic hypertension complicates between 1-5% of pregnancies and is associated with adverse outcomes including preterm delivery, superimposed pre-eclampsia, perinatal death, placental abruption and fetal growth restriction(4). The pathogenesis of chronic hypertension is multifactorial with increased peripheral vascular resistance, endothelial dysfunction, autonomic nervous system and renin-angiotensin-aldosterone system dysregulation. These factors may alter the venous return and thus susceptibility to SHS during MRI in the supine position.
In a previous study (5), we found that IVC morphology and IVC venous return is compromised in the supine position. However, venous return is increased in the spinal venous plexus maintaining vascular homeostasis.
The aim of this study was to use phase contrast (PC) quantitative flow imaging to assess differences in vessel morphology and venous return in chronic hypertensive and normotensive pregnant women in the supine position.
Methods
Participants
Sixteen pregnant participants underwent PC imaging of the IVC, aorta and spinal venous plexus in the supine position. Eight participants with chronic hypertension (foetal gestational age (GA) range: 20+5 weeks - 30+4 weeks, median, 23+6 weeks) were compared with eight foetal GA matched normotensive participants (foetal GA range 22+0 weeks - 30+2 weeks, median 24+4 weeks). Written informed consent was obtained prior to imaging. The chronic hypertensive cohort were all on antihypertensive medication, with aspirin as a common medication for all.
Imaging
Imaging was perrformed on a 3T Philips Achieva (Best, Netherlands) using a 32-channel cardiac coil at the Evelina New Born Imaging Centre, St Thomas Hospital, London, UK. The PC sequence parameters were: 2D FFE PC-flow (low SAR, low PNS) and reduced noise (<110dB), TR=5.7ms, TE 3.5ms, FOV=320X280X2.5mm, slice thickness=8mm, sense factor 2, time=12secs. The venc varied between 50-70cm/s as appropriate to prevent aliasing of the IVC and aorta. The sequence was performed on expiration in a transverse slice perpendicular to the spine at the level of L3/L4. Blood pressure (BP) was recorded throughout the examination. Each participant spent approximately 30mins in the supine position.
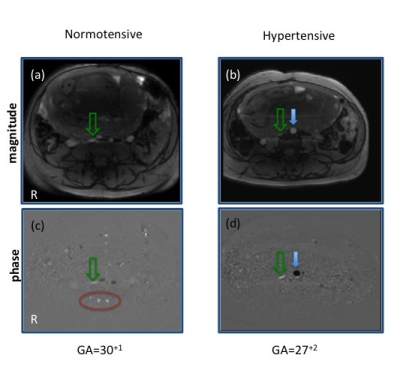
PC-flow analysis was performed using Medviso (Segment v2.0 (http:/segment.heiber.se). Regions of interest (ROI) were drawn around the IVC, (figure 1, green arrows), the spinal venous plexus, (figure 1, red circle) and the aorta (figure 1, blue arrow). Venous return (L/min) was determined by integrating the velocity across space and through time for each ROI. Morphology of the IVC was estimated by measuring the antero-posterior height of the IVC using ImageJ, v1.49 (National Institute of Health, USA).
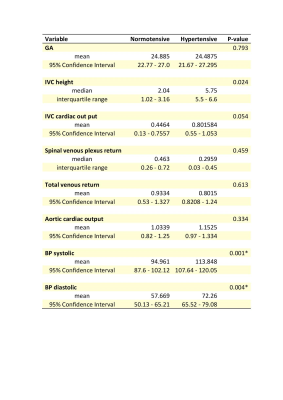
We compared (i) IVC height, (ii) IVC venous return, (iii) spinal venous plexus return, (iv) total venous return (IVC and spinal venous plexus), (v) aorta flow and (vi) systolic and (vii) diastolic blood pressure between the two groups. Statistical analysis was performed using SPSS v23, USA.
Differences between non-parametric variables (IVC height, spinal and venous plexus return) were assessed using a Mann-Whitney U Test. All other variables were parametric and were assessed using an independent samples t-test. Results were Bonferroni corrected for multiple comparisons (p=0.007).
Results
Participants in both groups tolerated the supine position well with no reported symptoms of SHS. The chronic hypertensive women had significantly greater systolic and diastolic BP than the normotensive women. However, venous return and IVC morphology in this group were not significantly different with the normotensive participants after Bonferroni correction (Table 1).Conclusions
These results suggest that chronic hypertensive pregnant women maintain venous return blood flow as effectively as normotensives and so can be
scanned in the supine position without greater risk of SHS. Acknowledgements
This work received funding from the European Research Council under the European Union’s Seventh Framework Programme [FP7/20072013]/ERC grant agreement no. 319456 (dHCP project), the NIH Human Placenta Project grant 1U01HD087202-01, and was supported by the Wellcome EPSRC Centre for Medical Engineering at Kings College London [WT 203148/Z/16/Z], MRC strategic grant MR/K006355/1 and by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
References
(1) Kienzl D, Berger-Kulemann V, Kasparin G, Brugger PC, Weber M, Bettelheim D, Pusch F, Prayer D. Risk of inferior venac cava compression syndrome during fetal MRI in the supine position- a retrospective analysis. J. Perinat. Med. 2014; 42(3): 301–306
(2) Wright L. Postural hypotension in late pregnancy. The supine hypotensive syndrome.Br Med J. 1962 Mar 17;1(5280):760-2.
(3) F. Holmes, Incidence of the supine hypotensive syndrome in late pregnancy. A clinical study in 500 subjects. 1960 DOI: 10.1111/j.1471-0528.1960.tb06987.x
(4) Bramham, Kate; Parnell, Bethany; Nelson-Piercy, Catherine; Seed, Paul T; Poston, Lucilla; Chappell, Lucy C. Chronic hypertension and pregnancy outcomes: systematic review and meta-analysis. 2015. BMJ : British Medical Journal, volume 348.
(5) Hughes E.J , Price A.N, , McCabe L. , Pegoretti Baruteau K. Hutter J, Carney O., Gaspar A S, Hajnal J.V, Rutherford M.A. Magnetic Resonance Imaging quantification of venous return in pregnant women: a comparison between supine and left lateral tilt position. International Society for Magnetic Resonance Imaging in Medicine, Singapore, 2016.
Figures