4506
Characterization of Human Prostate Cancer Using Tissue Sodium Concentration Measured from Sodium MRI1Western University, London, ON, Canada, 2London Health Sciences Center, London, ON, Canada, 3Robarts Research Institute, London, ON, Canada, 4Ontario Institute for Cancer Research, Toronto, ON, Canada
Synopsis
Over-treatment of prostate cancer is a significant problem in men’s healthcare. Development of non-invasive imaging tools for improved identification of prostate lesions can reduce over-treatment. We have built custom sodium MRI hardware to image and quantify tissue sodium concentration (TSC) in the human prostate. Sodium and multi-parametric MR images are co-registered to Gleason-graded post-prostatectomy histology, the current gold standard for prostate cancer lesion characterization. Our data shows a statistically significant, positive correlation of TSC with Gleason score. These data suggest that TSC measured by sodium MRI, in addition to multi-parametric MRI has utility for non-invasive characterization of prostate cancer.
Introduction
Over treatment of prostate cancer is a significant problem in the health care of men [1,2], which causes decreased quality of life for patients and increased financial costs for society [3,4]. The unreliability of Gleason grading due to uncertainties related to biopsy is a major concern for physicians leading to conservative decision making when assigning men to active surveillance or treatment. Improved imaging tools for reliable lesion identification can greatly improve this situation. This study was preformed to determine whether tissue sodium concentration (TSC), assessed using sodium MRI, is related to tumour grade in patients with biopsy-proven prostate cancer.
Methods
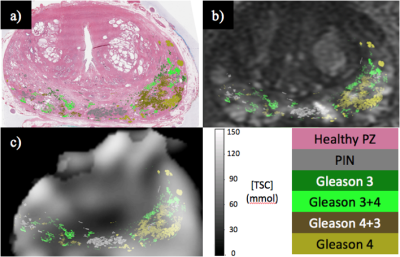
Imaging data were acquired from a cohort of ten men with biopsy-proven prostate cancer. In vivo multi-parametric MRI (Diffusion Weighted Imaging, T2-weighted imaging, Post-Gadolinium T1-weighted imaging) and sodium MR imaging were performed on patients prior to prostatectomy. Excised prostates were sectioned and then contoured by a pathologists’ assistant for Gleason grade prior to registration to the sodium images through a previously validated registration pipeline [5]. See figure 1 for an example of Gleason contours overlaid onto co-registered sodium and T2-weighted MR images. Sodium images were acquired with a custom build endorectal (ER) receive-only coil and an asymmetric transmit-only birdcage RF coil [6]. TSC data were normalized through a procedure developed by Axel et al. [7] to correct for the receive sensitivity profile of the ER receive coil.Results
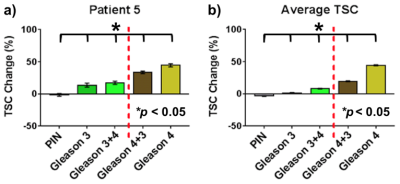
TSC was assessed in peripheral zone lesions as a change from healthy peripheral zone tissue as: [ ( TSCLesion - TSCHealthy )/ TSCHealthy ] x 100%. TSC measurements from a representative patient and the averaged TSC measurements for all patients is shown in figure 2. Statistically significant differences in TSC were measured between Gleason grades in the lesions of individual patients and in the average of all 10 patients. Furthermore, TSC changes in prostate lesions have shown a positive correlation with Gleason score.Discussion/Conclusion
These results suggest that TSC assessed by sodium MRI has utility to non-invasively characterize prostate cancer lesions. Our data shows a monotonic increase in TSC as Gleason score increases. The gold standard for prostate cancer diagnosis an invasive 12-core biopsy sampling less than 0.5% of the entire gland. Low-risk, Gleason 6 cancer is the most common diagnosis after biopsy; it rarely metastasizes and its associated mortality is almost zero. However, uncertainties due to negative biopsies or under-sampling of aggressive lesions is a major concern for physicians when assigning men to active surveillance. This leads to conservative management of men with low-risk disease who would otherwise be streamed to surveillance [8]. Increased patient confidence afforded by improved lesion detection and characterization using TSC in combination with multi-parametric MRI will reduce the psychological burden of living with untreated prostate cancer and tip the scales from treatment to active surveillance for low-risk disease.Acknowledgements
We would like to thank Peter Martin for assisting with the registration of histology to the mpMR images. We would thank Dave Reese for assisting with patient imaging. We would like to thank Mena Gaed for his work Gleason contouring the histology slides.References
[1] Rouse P. et al., Urologia Internationalis, 2011, 87(1), 49-53, [2] Djavan B. et al., Primary Care, 2010, 37(3), 441-459. [3] Dragomir A. et al., CMAJ Open, 2014, 2(2), E60-E68, [4] Eisemann N. et al., Qual Life Res, 2015, 24, 128-128. [5] Ward AD. et al., Radiology 2012, 263, 856–864. [6] Farag A. et al., J. Magn. Reson. Imaging 2015, 42, 436–445. [7] Axel L. et al., Amer J Roentgenol, 1987, 148, 418-420. [8] Morash C. et al., Cancer Care Ontario (CCO). 2014. S1, 2-6.Figures