4479
Assessing the Impact of Acid Aspiration with Hyperpolarized Xenon-129 Dissolved-Phase MRI1Radiology, University of Pennsylvania, Philadelphia, PA, United States
Synopsis
Acid aspiration frequently occurs in critically ill patients, and can give rise to severe acute lung injury. In this study, we investigated whether hyperpolarized xenon-129 dissolved-phase MRI provides the necessary sensitivity to assess acid aspiration and associated pneumonitis in a rabbit model. We observed changes that most likely corresponded to the formation of interstitial edema as part of an inflammatory response. In particular, perilesional areas of high xenon uptake may reflect tissue at risk of secondary ventilator-induced injury.
Purpose
Acid aspiration frequently occurs in critically ill patients, and can give rise to severe acute lung injury1. However, the effects of acid aspiration are often obscured by the development of ventilation-induced lung injury in mechanically-ventilated patients. In this study, we investigated whether hyperpolarized xenon-129 (HXe) dissolved-phase MRI provides the necessary sensitivity to assess acid aspiration and associated pneumonitis in a rabbit model.Methods
Imaging experiments were performed in 3 sedated New Zealand rabbits (approx. 4.5 kg). Animals were ventilated with room air until imaging began, at which point the gas mix was switched to 20% oxygen and 80% HXe for two breaths (6 ml/kg tidal volume). Mild lung injury was induced by instillation of 0.75 ml/kg of HCl into the right lung, followed by application of 4 cm positive end-expiratory pressure (PEEP) for 15 minutes. Imaging was performed at end inspiration, prior to and approximately 1 and 2 hours after injury. In one acquisition for one of the animals, a 5 cm PEEP was applied during imaging at the 2 hour time point. All studies were approved by the Institutional Animal Care and Use Committee. MR imaging was conducted using a 2D-projection gradient-echo sequence that employed a non-selective 900-μs Gaussian RF excitation pulse centered 3,530 Hz downfield from the gas-phase resonance. Taking advantage of the large frequency difference between the two phases, combined with a sufficiently small acquisition bandwidth, HXe in the pulmonary air spaces and dissolved in the lung tissue were imaged simultaneously, side-by-side2. The following sequence parameters were used: matrix size 32×80; TR 30, 100, or 200 ms; TE 2.7 ms; flip angle 40°; FOV 230 mm; receiver bandwidth 110 Hz/pixel. Ratios were calculated for a TR of 100 ms and 30 ms, as well as for a TR of 200 ms and 30 ms. All MR studies were performed at 1.5T (Avanto; Siemens), using a custom xenon-129 transmit/receive birdcage coil (Stark Contrast, Erlangen, Germany). Enriched xenon gas (87% xenon-129) was polarized using a prototype commercial system (XeBox-E10, Xemed LLC, Durham, NH).Results and Discussion
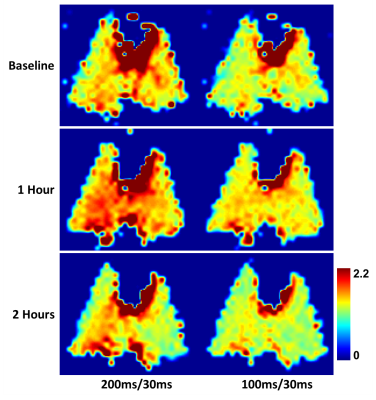
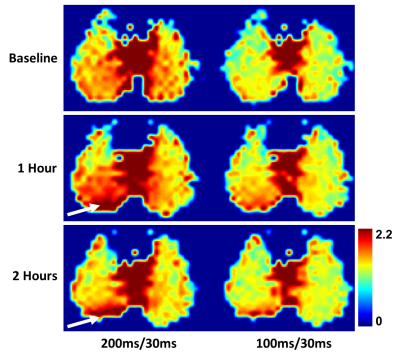
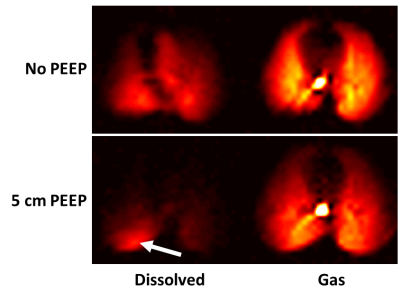
Figure 1 depicts the coronal dissolved-phase ratio maps prior to and following HCl administration. The 100 ms / 30 ms ratio is more heavily weighted towards upstream xenon uptake, while the 200 ms / 30 ms ratio is more reflective of downstream gas transport. At the one hour time point, the dissolved-phase ratios in the right lung appear elevated both compared to the baseline and relative to the left lung at the same time point. At 2 hours post-injury, the ratios have largely returned to baseline except for a channel-like structure ranging from the right main bronchus to the right base of the lung, which most likely highlights the volume of lung tissue that came in contact with the flowing acid. Corresponding axial maps are shown in Fig. 2: in this view it becomes apparent that most of the damage occurred in the posterior regions of the injured right lung, with a seemingly transitory response in the central lung region at 1 hour. The ratio maps further illustrate that the volume of the right lung is decreasing following acid administration, and that the lung volume immediately above the deflated region exhibits a large increase in xenon uptake (white arrows). The observed phenomenon is most likely caused by the formation of interstitial edema and a subsequent collapse of the lung parenchyma under its own weight. This assumption is supported by the acquisition with 5 cm PEEP (Fig. 3), which reopens the affected volume such that xenon gas can enter the injured region. Interestingly, xenon is only taken up by the edematous lung tissue at this pressure, while the rest of the lung exhibits little or no dissolved-phase signal. Finally, the absence of any xenon in the heart indicates that very little gas transport occurs at end inspiration under these conditions.Conclusion
We demonstrated that dissolved-phase HXe MRI is sensitive to the effects of acid aspiration, and that the detected changes in gas uptake most likely correspond to the formation of interstitial edema as part of an inflammatory response. In particular, perilesional areas of high xenon uptake may reflect tissue at risk of secondary ventilator-induced injury.Acknowledgements
Supported by NIH grants R01 EB015767 and R01 HL129805.References
[1] Raghavendran et al. Aspiration-Induced lung injury. Crit Care Med 2011;39(4):818-826.
[2] Mugler et al. Simultaneous magnetic resonance imaging of ventilation distribution and gas uptake in the human lung using hyperpolarized xenon-129. Proc Natl Acad Sci USA 2010;107(50):21707-21712.
Figures