4469
Clinical Translation of 3D Spiral-IDEAL for Single Breath-hold Imaging of Gas and Dissolved-Phase Hyperpolarized 129Xe in Human Lungs1Translational Medicine Program, Peter Gilgan Centre for Research and Learning, The Hospital for Sick Children, Toronto, ON, Canada, 2Department of Medical Biophysics, Univeristy of Toronto, Toronto, ON, Canada
Synopsis
Spiral-IDEAL is a fast and efficient technique for imaging dissolved-phase hyperpolarized 129Xe in tissue/blood plasma (T/P) and red blood cell (RBC) compartments of the lung. Previously, spiral-IDEAL has been limited to pre-clinical rodent models using multi-breath techniques not suitable for human subjects. In this work we optimize and demonstrate clinical translation of spiral-IDEAL for single breath-hold 129Xe imaging of human subjects. We compare and contrast several interleaved imaging strategies. Furthermore, we also demonstrate 3D spiral-IDEAL for simultaneous volumetric imaging of gas, T/P, and RBC compartments.
Introduction
Magnetic resonance imaging (MRI) of hyperpolarized (HP) 129Xe dissolved in the lung (i.e. tissue/plasma; T/P and red blood cells; RBCs) holds promise for evaluating diseases affecting gas exchange1. However, imaging the dissolved phases of 129Xe is challenging due to relatively low signal, short T2* (approximately 1.2ms for T/P and 0.9ms for RBC at 3T)2, and limited breath-hold duration tolerable by patients (10-20s). Several techniques for overcoming these difficulties have been successfully demonstrated in humans3–9. A technique for rapid spatial and spectral encoding known as spiral-IDEAL10 has previously been demonstrated by our group in rodents11–13. In this work we describe an approach based on interleaved spiral-IDEAL for breath-hold 3D imaging of gas and dissolved 129Xe in the lung and demonstrate preliminary results in healthy volunteers.Methods
Healthy volunteers were imaged with approval of the research ethics board at The Hospital for Sick Children after obtaining written consent. Imaging was performed on a clinical 3T scanner (Prisma, Siemens GmbH, Erlangen, Germany) with a flexible transmit/receive vest coil (Clinical MR Solutions, Brookfield, WI). For a gradient amplitude of 80mT/m, a slew rate of 199mT/m/ms, BW=100kHz, and FOV of 48×48cm2, several spiral trajectories with varying numbers of interleaves (Nint) were designed to optimize individual readout time (Tread), spatial resolution, and total acquisition time (Tacq). Spectral encoding was achieved by shifting echo times (TE) between k-space acquisitions (ΔTE=370μs) using four echoes. For localization in the z-direction, Cartesian phase-encoding was implemented in a stack-of-spirals fashion14. Isotopically enriched (~86%) 129Xe was hyperpolarized using a commercial polarizer (Model 9800, Polarean, Durham, NC) yielding a polarization of ~12%. Spiral gradient waveform design and image reconstruction were performed in MATLAB (MathWorks, Natick, MA).Results
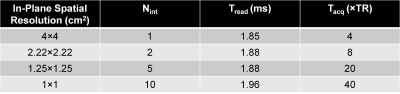
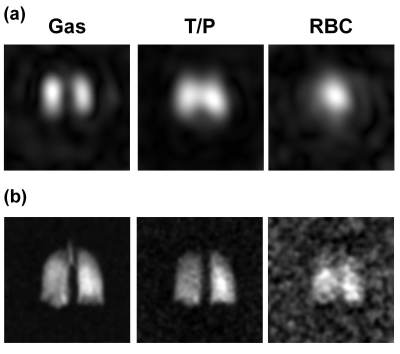
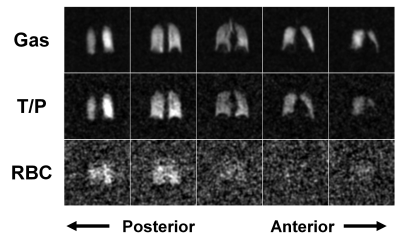
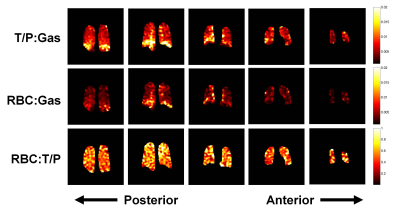
Table 1 shows a summary of investigated spiral trajectories, illustrating trade-offs between timing, nominal image resolution, and interleaves. Fig. 1 shows the two trajectories that were tested in-vivo while Fig. 2 shows representative human 2D coronal projections. A representative 3D image set using spiral-IDEAL in a stack-of-spirals fashion is shown in Fig. 3. Fig. 4 shows signal ratio maps for a set of coronal images.Discussion
In this work we demonstrate application of 3D spiral-IDEAL imaging of 129Xe in human subjects within a single breath-hold. Coronal 2D projections acquired using a single-shot spiral trajectory (Fig. 2a) showed good spectral decomposition. However, the low spatial resolution of the single-shot acquisition lead to blurry images that are difficult to resolve. This is especially true of the dissolved images (specifically RBC) which exhibit further blurring due to short T2*. Interleaved spirals allowed for improved spatial resolution while keeping Tread short (Fig. 2b). Stack-of-spirals implementation allowed for volumetric imaging of all three 129Xe resonances. Because k-space is encoded on a Cartesian grid in the z-direction, minimal reconstruction complexity is added. However, this comes at the expense of slightly increased initial TE due to the phase-encoding gradient (180μs) prior to acquisition.
Although interleaved spirals improved spatial resolution versus single-shot, they are increasingly time and RF intensive. The increased consumption of gas-phase magnetization due to the larger number of pulses requires further consideration. Some excitation of gas is desirable for normalization of dissolved signals (i.e. ventilation differences, T1 depolarization, RF history). However, over-excitation of the gas resonance depletes the overall magnetization available for transfer to the dissolved-phases, resulting in lower dissolved-phase signals. This is likely the reason for low RBC signal intensity in the coronal projections (Fig. 2b) and 3D images (Fig. 3). However in subsequent scans, dissolved signal was high enough to facilitate calculation of signal ratio maps which have been shown to be useful semi-quantitative measures of lung function (Fig. 4)5–9.
In future, optimization of excitation (i.e. increased spectral selectivity) should help improve image quality by reducing excitation of gas and increasing flip angle at the dissolved resonances. Furthermore, improvements to xenon polarization and the use of multi-channel radiofrequency coils will also help. Future work will involve further testing of the pulse sequence in healthy volunteers for optimization and application to patient populations (e.g. radiation-induced lung injury and bronchopulmonary dysplasia). Additionally, the flexibility of this sequence allows volumetric resolution to be traded for repeated imaging at multiple exchange times to quantify gas exchange regionally.
Conclusion
This work demonstrates the feasibility of performing 3D spiral-IDEAL imaging of dissolved phase HP 129Xe in human subjects within a breath-hold. This technique holds promise for rapid, quantitative imaging of dissolved 129Xe uptake, which may be particularly useful for the investigation of lung diseases which affect gas exchange.Acknowledgements
This work was supported by NSERC (RGPIN 217015-2013) and CIHR (MOP 123431). Special thanks to Nikhil Kanhere, Elaine Stirrat, Marcus Couch, Yonni Friedlander, Andras Lindenmaier, Ruth Weiss, and Tammy Rayner for assistance with imaging experiments. B.Z was supported by a Research Training Competition (RESTRACOMP) award from The Hospital for Sick Children.References
1. K. Ruppert, J.R. Brookeman, K.D. Hagspiel, B. Driehuys, and J.P. Mugler, “NMR of hyperpolarized 129Xe in the canine chest: Spectral dynamics during a breath-hold,” NMR Biomed. 13(4), 220–228 (2000).
2. Y. V Chang, J.D. Quirk, I.C. Ruset, J.J. Atkinson, F.W. Hersman, and J.C. Woods, “Quantification of human lung structure and physiology using hyperpolarized 129Xe,” Magn. Reson. Med. 71(1), 339–344 (2014).
3 . J.P. Mugler III, T.A. Altes, I.C. Ruset, et al., “Simultaneous magnetic resonance imaging of ventilation distribution and gas uptake in the human lung using hyperpolarized xenon-129.,” Proc. Natl. Acad. Sci. U. S. A. 107(50), 21707–12 (2010).
4. Z.I. Cleveland, G.P. Cofer, G. Metz, et al., “Hyperpolarized Xe MR imaging of alveolar gas uptake in humans.,” PLoS One 5(8), e12192 (2010).
5. K. Qing, K. Ruppert, Y. Jiang, et al., “Regional mapping of gas uptake by blood and tissue in the human lung using hyperpolarized xenon-129 MRI.,” J. Magn. Reson. Imaging 39(2), 346–59 (2014).
6. K. Qing, J.P. Mugler, T.A. Altes, et al., “Assessment of lung function in asthma and COPD using hyperpolarized 129Xe chemical shift saturation recovery spectroscopy and dissolved-phase MRI,” NMR Biomed. 27(12), 1490–1501 (2014).
7. S.S. Kaushik, S.H. Robertson, M.S. Freeman, et al., “Single-breath clinical imaging of hyperpolarized 129xe in the airspaces, barrier, and red blood cells using an interleaved 3D radial 1-point Dixon acquisition,” Magn. Reson. Med. 75(4), 1434–1443 (2016).
8. Z. Wang, S.H. Robertson, J. Wang, et al., “Quantitative analysis of hyperpolarized 129 Xe gas transfer MRI,” Med. Phys. 44(6), 2415–2428 (2017).
9. J.M. Wang, S.H. Robertson, Z. Wang, et al., “Using hyperpolarized 129 Xe MRI to quantify regional gas transfer in idiopathic pulmonary fibrosis,” Thorax (2017) [Published online ahead of print] http://thorax.bmj.com/lookup/doi/10.1136/thoraxjnl-2017-210070.
10. F. Wiesinger, E. Weidl, M.I. Menzel, et al., “IDEAL spiral CSI for dynamic metabolic MR imaging of hyperpolarized [1-13C] pyruvate,” Magn. Reson. Med. 68(1), 8–16 (2012).
11. O. Doganay, T. Wade, E. Hegarty, C. McKenzie, R.F. Schulte, and G.E. Santyr, “Hyperpolarized 129 Xe imaging of the rat lung using spiral IDEAL,” Magn. Reson. Med. 76(2), 566–576 (2015).
12. O. Doganay, E. Stirrat, C. McKenzie, R.F. Schulte, and G.E. Santyr, “Quantification of regional early stage gas exchange changes using hyperpolarized 129 Xe MRI in a rat model of radiation-induced lung injury,” Med. Phys. 43(5), 2410–2420 (2016).
13. B. Zanette, E. Stirrat, S. Jelveh, A. Hope, and G.E. Santyr, “Regional Detection of Lung Injury using Hyperpolarized Xenon-129 Mapping of Blood Hematocrit in a Rat Model Involving Partial-Lung Irradiation,” Proc. Intl. Soc. Mag. Reson. Med. 25(1184), (2017).
14. P. Irarrazabal and D.G. Nishimura, “Fast Three Dimensional Magnetic Resonance Imaging,” Magn. Reson. Med. 33(5), 656–662 (1995).
Figures