4452
Quantitative Predictors of Response to Neoadjuvant Chemotherapy on Dynamic Contrast-Enhanced Breast MRI1UCLA, Los Angeles, CA, United States
Synopsis
In this IRB-approved, HIPAA-compliant retrospective study, 63 consecutive women with newly diagnosed breast cancer undergoing neoadjuvant chemotherapy with pre- and post- chemotherapy breast MRI on a 3.0 Tesla scanner prior to surgery at our institution between January 2013 and December 2015 were included for analysis. Decrease in tumor size, decrease in peak enhancement, increase in time to peak, decrease in wash in, and decrease in wash out on post-chemotherapy breast MRIs were predictive of pathologic complete response on surgical pathology, a surrogate for prognosis.
Introduction
For locally advanced breast cancer, neoadjuvant chemotherapy before surgery is now the standard of care, both because it increases the likelihood of breast conserving surgery and because it provides prognostic information based on response to chemotherapy (1). On surgical pathology, the presence of complete pathologic response (pCR) is considered a good prognostic indicator for long term survival (2).
Dynamic contrast-enhanced breast magnetic resonance imaging (MRI) plays an important role in the staging of breast cancer, in the estimation of disease burden, and in predicting response to chemotherapy (3, 4). MRI has been lauded for its increased sensitivity compared to other breast imaging modalities such as mammography and sonography, however it has also been criticized for its relatively low specificity, leading to false positives that necessitate additional imaging and biopsies prior to treatment, adding to treatment delays and patient anxiety.
Traditionally, the morphology of imaging findings on MRI has trumped contrast kinetic features. More recently, and especially in applications of MRI outside breast cancer such as in prostate cancer, quantitative imaging parameters such as peak enhancement, time to peak enhancement, wash in, wash out, Ktrans, and kep have played an essential role in contributing to the detection and assessment of imaging findings.
The purpose of this study was to determine whether quantitative imaging parameters on pre-chemotherapy breast MRI, post-chemotherapy breast MRI, or both could predict pCR.
Methods
In this IRB-approved, HIPAA-compliant, retrospective study, institutional databases were search for consecutive women with newly diagnosed breast cancer undergoing neoadjuvant chemotherapy with pre- and post- chemotherapy breast MRI on a 3.0 Tesla scanner prior to surgery at our institution between January 2013 and December 2015 were included for analysis.
Maximal dimensions of disease were measured and quantitative parameters based on manual ROIs drawn on first post-contrast T1 sequences were determined using software (Olea Medical, La Ciotat, France).
Surgical pathology reports were used to determine presence or absence of pCR. Differences in quantitative parameters in women with pCR versus women with no pCR were assessed using logistic regression analysis. A P value < 0.05 was significant.
Results
63 women with a mean age of 49 years at pre-chemotherapy breast MRI (range, 26 to 74 years) were included for analysis. 31 were pre-menopausal, and 32 were post-menopausal. Risk factors for breast cancer included 18 instances of gene mutations (10 BRCA, 8 other such as ATM and CHEK 2), two instances of personal high risk lesion such as atypical ductal hyperplasia, and 10 instances of first degree family relative with breast cancer.
29 women had invasive ductal carcinoma (IDC) (one grade 1, three grade 2, 25 grade 3), 29 had with IDC with ductal carcinoma in situ (DCIS) (one grade 1, nine grade 2, 19 grade 3), three had other invasive subtype (1 grade 2, 2 grade 3), and two had DCIS (1 grade 3, 1 unknown). Six women had stage 1 disease, 34 had stage 2, and 23 had stage 3. The majority of women had scattered fibroglandular tissue (34 of 63) and mild background parenchymal enhancement on pre-chemotherapy breast MRI (26 of 63). There were 56 instances of masses, 26 of NME, and 14 of foci, with mean maximal dimension of disease measuring 44 mm (range, 10-110 mm). The majority of women underwent taxotere/carboplatin/Herceptin with or without Perjeta (26 of 63). 29 women had pCR on surgical pathology, and 34 had no pCR.
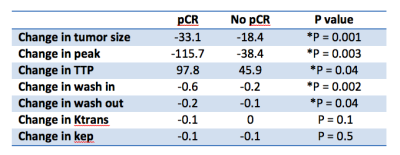
On pre-chemotherapy breast MRI, women with pCR versus no pCR had similar mean peak enhancement (167.6 versus 176.5), mean time to peak (TTP) (225.1 versus 220.2), mean wash in (0.8 for both), mean wash out (0.2 for both), mean Ktrans (0.2 for both), and mean kep (0.4 versus 0.5), respectively. Comparing post-chemotherapy to pre-chemotherapy quantitative parameters, women with pCR had a greater mean decrease in tumor size (-33.1 versus -18.4, p = 0.001), a greater mean decrease in peak enhancement (-115.7 versus -38.4, p = 0.003), a mean increase in time to peak (97.8 versus 45.9, p = 0.04), a greater decrease in wash in (-0.6 versus -0.2, p = 0.002), a greater decrease in wash out (-0.2 versus -0.1, p = 0.04), a greater decrease in Ktrans (-0.1 versus 0.0), and the same mean change in kep (-0.1 for both).
Discussion/Conclusion
In this study, quantitative parameters on pre-chemotherapy breast MRI were unable to distinguish women who would have pCR from those who would have no pCR, however changes in these quantitative parameters on post-chemotherapy breast MRIs were highly predictive of women who would have pCR. In clinical practice, this study suggests that women would benefit from MRI both at the beginning and end of chemotherapy for prognostic information.Acknowledgements
No acknowledgement found.References
1. van der Hage JA, van de Velde CJ, Julien JP, Tubiana-Hulin M, Vandervelden C, Duchateau L. Preoperative chemotherapy in primary operable breast cancer: results from the European Organization for Research and Treatment of Cancer trial 10902. J Clin Oncol 2001; 19:4224-4237 2.
2. Rastogi P, Anderson SJ, Bear HD, et al. Preoperative chemotherapy: updates of National Surgical Adjuvant Breast and Bowel Project Protocols B-18 and B-27. J Clin Oncol 2008; 26:778-785 3.
3. Uematsu T, Kasami M, Yuen S. Neoadjuvant chemotherapy for breast cancer: correlation between the baseline MR imaging findings and responses to therapy. Eur Radiol 2010; 20:2315-2322