4381
Preliminary Investigation of MR Elastography to Predict Lymph Node Metastasis in Prostate Cancer1Department of Radiology, the Third Affiliated Hospital of Sun Yat-sen University(SYSU), Guangzhou, China, 2Department of Radiology, Mayo Clinic, Rochester, MN, United States, 3Department of Urology, the Third Affiliated Hospital of Sun Yat-sen University(SYSU), Guangzhou, China
Synopsis
Prostate cancer(PCa) is one of the leading causes of cancer-related deaths in North American men. Nodal metastases occur in 3-42% of men with clinically localized prostate cancer and the presence of nodal metastases has a strong negative impact on survival. Lymph node staging plays an important role in planning initial management in nonmetastatic PCa. Early detection and resection are important for staging and for the prognosis. We evaluated the diagnostic performance of MR elastography (MRE) in patients with PCa. Results from 33 patients with PCa show that MRE at both of 60Hz and 90Hz has the potential to be a useful technique for predicting PCa lymph node metastases and to establish prognosis and treatment planning.
Introduction
Prostate cancer (PCa) is one of the most common cancers in men and the global burden of this disease is rising1. Lymph node metastasis(LNM) is an essential prognostic factor in patients with prostate cancer2, 3. Curative treatment by radical prostatectomy(RP) or radical radiotherapy is no longer the optimal treatment in patients with pelvic LNM4. Preoperative prediction of LNM could help identify treatment options and predict prognosis. CT and MRI cannot reliably detect small LNM and enlarged lymph nodes due to hyperplasia that may cause false positives5-8. The stiffness of malignant human prostate tissue has been reported to be approximately 2–3-fold greater than normal or benign tissues in ex vivo measurements, which suggests that the biomechanical properties of prostate tissue may be useful as an independent diagnostic parameter9-12. The aim of this study was to assess the diagnostic feasibility of MR elastography (MRE) for the identification of PCa LNM in patients undergoing RP and extended pelvic lymph node dissection (ePLND).Methods
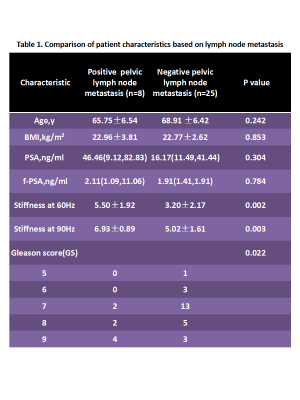
An institutional review board approved database of 57 patients pathologically confirmed as having PCa after RP who gave written consent and underwent 3D SE-EPI MRE was retrospectively reviewed. 24 patients were excluded from this pilot study due to the lack of ePLND (N=14), locoregional therapy(N=6), or the MRE information in the PCa was unsatisfactory for analysis(N=4). The remaining 33 patients were enrolled in this study. Clinical parameters included prostate serum antigen (PSA), free-prostate serum antigen(fPSA), and Gleason score were recorded. PCa was indicated on T2-weighted images with biopsy results as the reference standard and subjects were stratified into two groups based on regional LNM: group 1 = negative regional LNM (N=25), and group 2 = positive regional LNM(N=8)(Table 1). MRE was performed on a 3.0T scanner(GE, Discovery MR750, Waukesha, WI) with a free-breathing, multislice, single-shot, flow-compensated, spin-echo, EPI, 3D-MRE sequence using 60-Hz and 90-Hz vibrations. The acquisition parameters included acquisition matrix = 80x80; parallel imaging factor = 2;TR/TE =1555.7-1667.2/48.0-56.3ms; 4 time steps; scan time = 40 sec; 24-cm FOV; 20 3-mm axial slices with 1-mm gap; and through-plane motion encoding with bipolar, 6.45-ms, 50-mT/m motion-encoding gradients on each side of the refocusing pulse. A pelvic wall passive driver, developed by Mayo Clinic, was applied to the lower abdominal wall, partially overlapping the symphysis pubis. The MRE magnitude and phase images were processed using a 3D direct inversion (DI) of the Helmholtz wave equation using the curl of the MRE-measured wave field to calculate the stiffness. Regions of interest(ROIs) were drawn in the PCa area, and were adjusted to exclude prostate edges, significant wave interference, and any other artifacts seen on the magnitude and phase images. The mean prostate stiffness (in kiloPascals (kPa)) within the ROIs was recorded. Clinical pathology data were compared between the two groups using an independent-samples t-test. Receiver operating characteristic(ROC) analysis was performed to assess the diagnostic performance of prostate stiffness at each frequency for evaluating regional LNM. Statistical significance was defined as P<0.05.Results
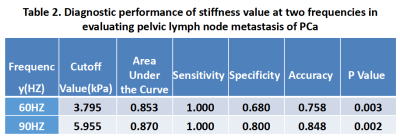
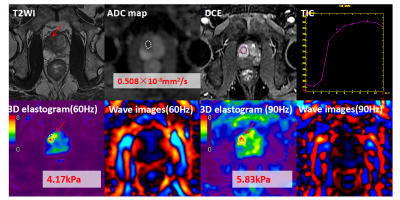
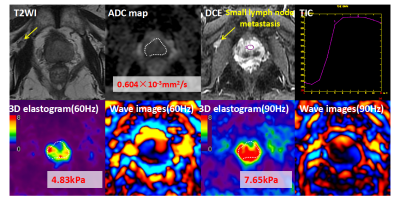
Baseline variables, including age, BMI, serum PSA and fPSA were similar between the two groups (P>0.05). PCa with pelvic LNM were significantly associated with high Gleason score (P=0.022). Gleason score was positively correlated with the PCa stiffness at 60Hz(r=0.365, P=0.037 ) and 90Hz(r=0.487, P=0.005). PCa with LNM (N=8) were significantly stiffer than without pelvic LNM (N=25) at both 60Hz(p=0.002) and 90Hz(P=0.003)(Figures 1 and 2). The most accurate cut-off level of for discriminating PCa with and without LNM was 3.795kPa at 60 Hz (0.853) and 5.955kPa at 90 Hz (0.870). The difference between the AUROCs was not significant (P=0.7736)(Table 2). The diagnostic accuracy, sensitivity, and specificity of MRE at 60 Hz and 90Hz were75.8% and 84.8%, 68% and 80%, and 100% and 100%, respectively.Discussion
MRE is a noninvasive, quantitative method that can detect changes in tissue biomechanics brought about by disease, such as cancer and fibrosis13, 14. Conventional imaging techniques, such as CT and MRI, rely on size criteria to determine lymph node status, and since metastatic nodes in prostate cancer usually are small, the sensitivity of these techniques is low (30%)8. Our results show PCa with pelvic LNM is significantly stiffer than without LNM. Our study demonstrated that MRE has the potential to provide PCa stiffness information and information about the frequency dispersion of tissue mechanical properties that may be useful for predicting PCa LNM preoperatively and noninvasively.Conclusion
MRE has the potential for predicting PCa lymph node metastases may be a useful tool to improve PCa prognosis and treatment planning.Acknowledgements
No acknowledgement found.References
1. Cuzick J, Thorat MA, Andriole G, et al. Prevention and early detection of prostate cancer. Lancet Oncol. 2014; 15:e484-92.
2. Cagiannos I, Karakiewicz P, Eastham JA, et al. A preoperative nomogram identifying decreased risk of positive pelvic lymph nodes in patients with prostate cancer. J Urol. 2003; 170:1798-803.
3. Hricak H, Schoder H, Pucar D, et al. Advances in imaging in the postoperative patient with a rising prostate-specific antigen level. Semin Oncol. 2003; 30:616-34.
4. Cheng L, Zincke H, Blute ML, et al. Risk of prostate carcinoma death in patients with lymph node metastasis. Cancer. 2001; 91:66-73.
5. Chang SS. Re: Metastases in Normal-Sized Pelvic Lymph Nodes: Detection with Diffusion-Weighted MR Imaging. J Urol. 2015; 194:954-5.
6. Thoeny HC, Froehlich JM, Triantafyllou M, et al. Metastases in normal-sized pelvic lymph nodes: detection with diffusion-weighted MR imaging. Radiology. 2014; 273:125-35.
7. Bader P, Burkhard FC, Markwalder R, et al. Is a limited lymph node dissection an adequate staging procedure for prostate cancer? J Urol. 2002; 168:514-8.
8. Turkbey B, Pinto PA, Mani H, et al. Prostate cancer: value of multiparametric MR imaging at 3 T for detection--histopathologic correlation. Radiology. 2010; 255:89-99.
9. Arani A, Plewes D, Krieger A, et al. The feasibility of endorectal MR elastography for prostate cancer localization. Magn Reson Med. 2011; 66:1649-57.
10. Wang J, Zhang TH, Glaser KJ, et al. Clinical Evaluation of a Simple Approach for Improving Shear Wave Illumination in Magnetic Resonance Elastography of the Prostate. Honolulu, ISMRM. Number:5786.
11. Zhang TH, Wang J, Glaser KJ, et al. Magnetic Resonance Elastography of the Prostate: Impact of Driver Size on Image Quality. Honolulu, ISMRM. Number:5930.
12. Wang J, Glaser KJ, He BJ, et al. MR Elastography of The Prostate with A Mode-Conversion Endourethral Driver Feasibility at 3.0 T. Singapore, ISMRM. Number:2760.
13. Venkatesh SK, Ehman RL. Magnetic resonance elastography of abdomen. Abdom Imaging. 2015; 40:745-59.
14. Pepin KM, Ehman RL, McGee KP. Magnetic resonance elastography (MRE) in cancer: Technique, analysis, and applications. Prog Nucl Magn Reson Spectrosc. 2015; 90-91:32-48.
Figures