4378
Feasibility of USPIO enhanced 7 Tesla MRI for detecting lymph node metastases in prostate cancer1Radiology and Nuclear Medicine, Radboud University Medical Centre Nijmegen, Nijmegen, Netherlands, 2Erwin L. Hahn Institute for MR Imaging, University of Duisburg-Essen, Essen, Germany
Synopsis
Ultrahigh field MRI offers opportunities for USPIO enhanced MRI for diagnosing lymph node metastases in prostate cancer, by improving resolution and increasing the sensitivity to USPIO particles. The assessment of lymph nodes based on size, shape and USPIO uptake can improve the differentiation between non-cancer and metastatic lymph nodes and may also lower the detection size limit for metastatic nodes. In this work we show the first results of USPIO enhanced MRI and computed echo time imaging of patients with high risk prostate cancer at 7 Tesla.
Introduction
Lymph nodes often are the first station of
metastasis in prostate cancer and it is important to detect them at an early
stage. Ultrasmall superparamagnetic iron oxide (USPIO) enhanced MRI is a
technique to diagnose pelvic lymph node metastases (1,2). The particles accumulate in
healthy lymph node tissue, resulting in significant signal loss on strongly
T2*-weighted (T2*W) imaging. Parts of the lymph node that contain metastases
from prostate cancer do not accumulate USPIOs and will therefore retain MR
signal intensity. By performing USPIO enhanced MRI on a higher field strength,
signal-to-noise and therefore resolution can be improved. In addition, the
susceptibility effect of USPIOs becomes stronger on higher field strengths.
This offers opportunities, because it might allow the detection of smaller
lymph nodes metastases and improve the differentiation between healthy lymph
nodes and metastases.
In this abstract we show the feasibility of USPIO enhanced MRI for detecting
pelvic lymph node metastases of prostate cancer on a 7 Tesla MRI system.
Methods
Patients with high risk prostate cancer were scanned 24-36 hours after a USPIO (ferumoxtran-10) dose of 2.6 mg iron per kg of bodyweight, which was dissolved in 100cc saline and administered intravenously over a period of 30-45 minutes. In addition, they received an intramuscular dose of scopolamine butylbromide just before the MRI scan.
A 7T whole body MR system (Magnetom 7T, Siemens Healthcare, Erlangen, Germany) was used with an 8 channel 1H transceiver body-array coil with meander-type microstrip elements (3). After B0 and B1+ shimming, water and lipid selective imaging was performed using the TIAMO (4) technique to obtain homogeneous body imaging. The scanned area contained at least the area from the aortic bifurcation to the base of the bladder.
Lipid selective imaging was performed with a 3D gradient echo (GRE) sequence with a TE of 2.09 ms, TR of 5.2 ms, voxel size of 0.66x0.66x0.66 mm3 (FOV 210x210x169 mm3, matrix 320x320x256) and acquisition time of 2 minutes and 51 seconds. Water-selective imaging was performed using a 3D multi-GRE sequence with a 970 µs water selective block pulse, TR of 14 ms, voxel size of 0.66x0.66x0.66 mm3 (FOV 210x210x169 mm3, matrix 320x320x256), acquisition time of 8 minutes and 23 seconds and multiple T2* weighted contrasts (TE of 2.10, 4.19, 6.21, 8.30 and 10.32 ms), from which computed TE images were reconstructed using a weighted linear least squares fitting procedure (5,6).
Results
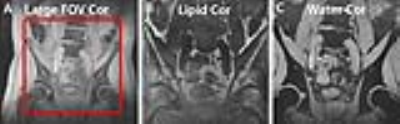
Data from two patients is shown in this work. The lipid- and water selective T2*W images feature a high resolution and separate lipid and water signals well. No substantial B1+ inhomogeneities were noticed using the TIAMO technique (Figure 1). The lipid-selective sequence allows the detection of normal USPIO rich lymph nodes, due to the bright lipid background. The high resolution water-selective imaging allows lymph nodes to be assessed on shape and size in three different orientations (Figure 2).The computed echo time imaging enables the choice of TE and T2*W and can be used to separate lymph nodes with and without USPIO uptake. Particularly, the extrapolated TE=18ms image shows a completely black lymph node with USPIO uptake, whereas the suspicious lymph node still appears bright on the same image set. This is also reflected by the R2* map.
Discussion
Our results show that imaging of the pelvis on 7 Tesla MRI is feasible at a high spatial resolution, enabling an accurate evaluation of lymph node size and shape. In addition, it may allow the detection of smaller lymph node metastasis. Moreover, the susceptibility of USPIO particles should result in larger R2* values on ultrahigh field. Computed TE imaging, including the R2* map, provides the tools to optimize TE and to quantitatively assess USPIO uptake, such that differentiation between normal lymph nodes and metastases can be optimized. Additional clinical studies need to be performed to assess how these technical advances translate to clinic.Conclusion
USPIO enhanced MRI for detecting lymph node metastases in prostate cancer is feasible at 7 Tesla and allows high resolution and computed echo time imaging.Acknowledgements
Dutch Cancer Society [2014-6624]References
1. Heesakkers RA, Jager GJ, Hovels AM, de Hoop B, van den Bosch HC, Raat F, Witjes JA, Mulders PF, van der Kaa CH, Barentsz JO. Prostate cancer: detection of lymph node metastases outside the routine surgical area with ferumoxtran-10-enhanced MR imaging. Radiology 2009;251(2):408-414.
2. Harisinghani MG, Barentsz J, Hahn PF, Deserno WM, Tabatabaei S, van de Kaa CH, de la Rosette J, Weissleder R. Noninvasive detection of clinically occult lymph-node metastases in prostate cancer. N Engl J Med 2003;348(25):2491-2499.
3. Orzada S, Quick HH, Ladd ME, Bahr A, Bolz T, Yazdanbakhsh P, Solbach K, Bitz AK. A flexible 8-channel transmit/receive body coil for 7 T human imaging 2009; Honolulu, Hawaii, USA. p 2999.
4. Orzada S, Maderwald S, Poser BA, Bitz AK, Quick HH, Ladd ME. RF excitation using time interleaved acquisition of modes (TIAMO) to address B1 inhomogeneity in high-field MRI. Magn Reson Med 2010;64(2):327-333.
5. Philips BWJ, Fortuin AS, Orzada S, Scheenen TWJ, Maas MC. High resolution MR imaging of pelvic lymph nodes at 7 Tesla. Magn Reson Med 2017;78(3):1020-1028.
6. Veraart J, Sijbers J, Sunaert S, Leemans A, Jeurissen B. Weighted linear least squares estimation of diffusion MRI parameters: strengths, limitations, and pitfalls. Neuroimage 2013;81:335-346.
Figures