4371
Multi-parametric MRI features and pathologic outcome of wedge shaped lesions on T2-weighted images1Department of Radiology, University of Chicago, Chicago, IL, United States, 2Department of Radiology, Bezmialem Vakif University, Istanbul, Turkey, 3Department of Pathology, University of Chicago, Chicago, IL, United States
Synopsis
This study investigated the multi-parametric MRI features and pathologic outcome of wedge shaped lesions on T2-weighted images in 76 patients. A greater percentage of wedge shaped features were found to be malignant than shown previously. Malignant wedge shaped regions were primarily highly hypointense on ADC maps and showed early enhancement on DCE-MRI. Benign wedge shaped lesions were predominantly mildly hypointense on ADC maps and showed no early enhancement and pathologically outcome showed prostatitis, hemosiderin-laden macrophages, prominent blood vessels, intraluminal blood and atrophy. Malignant wedge shaped lesions were found to have significantly lower ADC compared to benign wedge shaped regions.
Introduction
Wedge shaped regions of hypointensity on T2-weighted (T2W) images are among the many pitfalls in prostate cancer (PCa) detection using multiparametric MRI (mpMRI). Wedge shaped hypointense region with indistinct margins on T2W images in the peripheral zone are generally associated with prostatitis, atrophy or fibrosis, and assigned a PIRADS score 2 indicating a low likelihood for malignancy (1). There is no clear consensus regarding the pathologic outcomes of wedge shaped feature and their appearance on mpMRI. Therefore, this study investigates the multi-parametric MRI (mpMRI) features and pathologic outcome of wedge shaped lesions on T2-weighted (T2W) images.Methods
Seventy-six patients with histologically confirmed PCa underwent preoperative MRI with a 3T Philips Achieva MR system prior to undergoing radical prostatectomy. Two radiologists were blinded to pathology results and worked in consensus to mark wedge shaped regions of hypointensity on T2W images. The appearance on mpMRI: apparent diffusion coefficient (ADC) maps (degree of hypointensity) and dynamic contrast enhanced (DCE) MRI (whether they show early enhancement) was assessed. The pathologic outcome of wedge shaped regions was assessed by matching MR images with whole mount histology retrospectively. Quantitative ADC values for the wedge shaped regions were measured. The difference in ADC values between malignant and benign wedge shaped lesions were assessed using a two tailed t-test. Receiver operating characteristics (ROC) analysis was performed to evaluate the performance of quantitative ADC values in distinguishing benign and malignant wedge shaped features.Results
Thirty-five wedge shaped regions were identified by the radiologists, of which 12 (34%) were found be malignant. Of the malignant wedge shaped lesions, one lesion was Gleason 3+3, seven were Gleason 3+4, three were Gleason 4+3, and one was Gleason 4+5. An investigation of the pathologic outcomes of the benign features showed that prostatitis: acute inflammation (7/23 = 30.4%) and chronic inflammation (9/23 = 39.1%), hemosiderin-laden macrophages (6/23 = 26.1%), prominent blood vessels (7/23 = 30.4%), intraluminal blood (6/23 = 26.1%) and atrophy (6/23 = 26.1%) were the common histological features in the benign wedge shaped regions (see Figure 3).
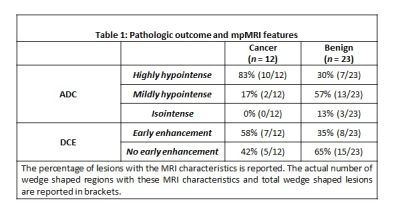
A majority of malignant wedge shaped regions were highly hypointense (10 out of 12 = 83%) on ADC maps and showed early enhancement on DCE-MRI (7 out of 12 = 58%). Whereas, the benign wedge shaped lesions were predominantly mildly hypointense (13/23 = 57%) on ADC maps and showed no early enhancement (15 out of 23 = 65%). The imaging characteristics of the wedge shaped lesions: benign and malignant on mpMRI are detailed in Table 1. Figures 1 and 2 show representative example of malignant and benign wedge shaped lesions on T2W images and their appearance on mpMRI: ADC maps and DCE-MRI.
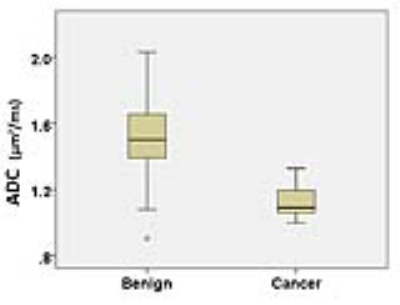
Malignant wedge shaped regions (1.13±0.11 µm2/ms) were found to have significantly lower (p = 0.0001) quantitative ADC values compared to benign wedge shaped regions (1.52±0.27 µm2/ms) (Figure 4). ROC analysis shows an AUC of 0.90 (p = 2.4×10-4, 95% confidence interval [0.79, 1.00]) for differentiating malignant and benign prostate tissue using quantitative ADC values.
Discussion
A greater percentage of wedge shaped features were found to be malignant than shown in previously published literature (2). However, pathologic outcomes in the previous study pathology results were based on systematically 12 core needle biopsies of the whole prostate and only T2W imaging was utilized. The lack of whole mount histology and mpMRI correlate in the earlier study highlights that biopsies can miss numerous cancers compared to the reference standard histology from prostatectomy specimens, while mpMRI is effective in predicting the pathologic outcome of wedge shaped lesion.
The wedge shaped lesions were commonly attributed primarily to prostatitis (1). While prostatitis is the most common pathologic outcome, other features hemosiderin-laden macrophages, prominent blood vessels, intraluminal blood and atrophy can also manifest as wedge shaped lesions.
Wedge shaped lesions on T2W images are assigned a PIRADS score 2 indicating a low likelihood for malignancy (1). However, since a greater percentage of wedge shaped features were found to be malignant, mpMRI (specifically quantitative ADC values) should be used to predict the pathologic outcome of wedge lesions on T2-weighted images, with significantly lower quantitative ADC values associated with presence of PCa, and therefore improving the interpretation of prostate mpMRI.
Conclusion
This study shows that greater percentage of wedge shaped features are malignant than previously thought. Benign conditions such as prostatitis (acute and inflammation), hemosiderin-laden macrophages, prominent blood vessels, intraluminal blood and atrophy can create wedge region on T2W-MRI. Importantly, mpMRI (specifically ADC) can distinguish between malignant and benign wedge shaped features.Acknowledgements
The study was funded by Philips Healthcare and National Institutes of Health (NIH R01 CA172801 and NIH 1S10OD018448-01).References
1. Weinreb JC, Barentsz JO, Choyke PL, Cornud F, Haider MA, Macura KJ, Margolis D, Schnall MD, Shtern F, Tempany CM, Thoeny HC, Verma S. PI-RADS Prostate Imaging – Reporting and Data System: 2015, Version 2. European Urology 2016;69(1):16-40.
2. Cruz M, Tsuda K, Narumi Y, Kuroiwa Y, Nose T, Kojima Y, Okuyama A, Takahashi S, Aozasa K, Barentsz J, Nakamura H. Characterization of low-intensity lesions in the peripheral zone of prostate on pre-biopsy endorectal coil MR imaging. European Radiology 2002;12(2):357-365.
Figures