4370
How often is the Dynamic Contrast Enhanced (DCE) score needed in PI-RADS version 2?1Radiology, Stanford University, Stanford, CA, United States, 2Urology, Stanford University, Stanford, CA, United States
Synopsis
The value of the Dynamic Contrast Enhanced (DCE) sequence in scoring a prostate lesion using PI-RADS version 2 is unknown. Our retrospective review of 213 patients who underwent prostate MRI and subsequent biopsy determined that the rate at which DCE was needed for obtaining the final PI-RADS score was 9%. This low rate raises the possibility of limiting the initial screening prostate MRI to an abbreviated non-contrast protocol, calling back the patient for the DCE sequence only if the initial exam is equivocal.
Introduction
Prostate Imaging Reporting And Data System (PI-RADS) version 2 assigns Diffusion-Weighted Imaging (DWI) as the dominant score for assessing prostate lesions in the peripheral zone and T2-weighted imaging (T2) as the dominant score in the transition zone. This change relegates Dynamic Contrast Enhanced (DCE) to a minor role; its primary value is to upstage peripheral-zone DWI scores of 3 to summary scores of 4 if DCE is positive [1]. The purpose of our study is to determine the rate at which DCE is needed in PI-RADS version 2.Methods
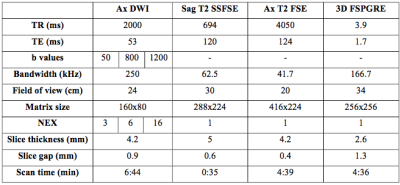
Our retrospective review of 213 patients was approved by the Institutional Review Board (IRB). Patients who underwent prostate MRI (Table 1) and subsequent prostate biopsy from January to December 2016 (one year) were included in our study. Prostate biopsy consisted of 12-core systematic biopsies, and MRI ultrasound fusion guided biopsy for patients with lesions on MRI. Patients with previous treatment for prostate cancer were excluded.
For each patient, age, Prostate-Specific Antigen (PSA) levels, and number of prostate lesions were recorded. For each prostate lesion, zone location, size, PI-RADS version 2 scores (T2, DWI, DCE, and summary), and biopsy results (Gleason score) were collected. Imaging findings from the clinical radiology report were used for our study and were not re-assessed.
The primary outcome of our study was the rate at which DCE was needed in PI-RADS version 2. DCE was deemed necessary if a peripheral-zone lesion had a DWI score of 3, or in the advent of DWI technical failure if a transition-zone lesion had a T2 score of 3. Secondary outcomes included the rate at which DCE positivity upstaged prostate lesions to PI-RADS 4 and the laboratory/pathology correlation of these equivocal lesions.
Results
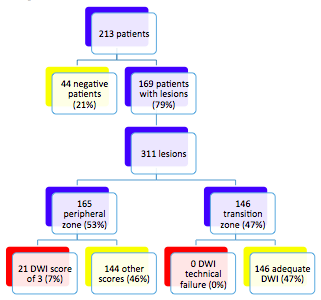
The mean age of our patients was 65 years, with mean PSA level of 9.0 ng/mL. Of our 213 patients, 44 did not have a prostate lesion (21%). In the remaining 169 patients, there were 311 prostate lesions (Figure 1), 165 of which being in the peripheral zone (53%). Twenty-one peripheral-zone lesions (7%) in 19 patients (9%, with a 90% confidence interval of 6-13%) had DWI scores of 3, requiring the DCE sequence. Of the 146 transition-zone lesions (47%), none had DWI technical failure to require DCE.
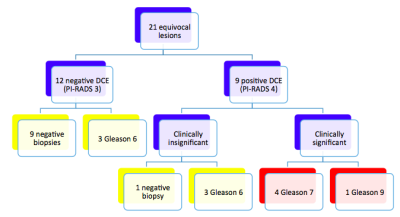
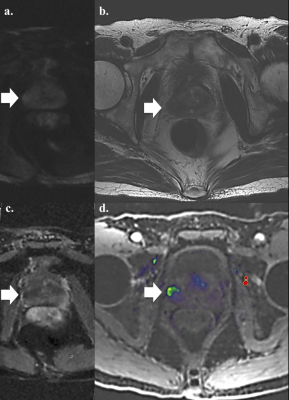
Of the 21 equivocal prostate lesions (Figure 2), nine were upstaged from PI-RADS 3 to 4 due to DCE positivity (Figure 3). There was no statistical difference in PSA levels between patients with negative and positive DCE (6.2 and 7.9 ng/mL, respectively; p=0.24). Five upstaged lesions were clinically significant with Gleason scores of 7 or higher. The remaining four upstaged lesions and 12 PI-RADS 3 lesions were clinically insignificant (ten negative biopsies and six Gleason scores of 6).
Discussion
Of our 213 patients, only 19 patients (9%) required the DCE sequence to score prostate lesions using PI-RADS version 2, potentially obviating intravenous contrast in the remaining 91%. This low rate of need for DCE raises the possibility of limiting the initial screening MRI to an abbreviated non-contrast exam with only T2 and DWI sequences. If the initial exam is then equivocal, the patient may then return for the DCE sequence (similar to the process of calling back patients after positive mammography in breast cancer screening or after positive low-dose chest CT in lung cancer screening). If an institution routinely targets all PI-RADS 3 lesions for biopsy (as is done at our institution), lesion upstaging would have no clinical significance and callbacks would only be needed for DWI failure.
The benefits of a limited screening prostate MRI include avoiding the nonzero risks associated with intravenous contrast, decreasing scan time with the abbreviated protocol, and decreasing the level of ancillary staff/monitoring needed for contrast exams. A potential risk is losing patients between the initial non-contrast MRI and any necessary follow-up DCE exams. Additionally, the DCE sequence may improve the overall sensitivity of lesion detection on MRI, a question that requires further study [2-4].
The limitations of our study include its retrospective study design and relatively small sample size. Due to our inclusion criteria, the rate of 9% of patients needing DCE is likely an overestimation, since patients with negative prostate MRI do not always undergo subsequent biopsy at our institution (excluding them from our study). Cost analysis is also needed to determine whether it is financially- and time-efficient to implement a process with shorter initial screening exams but with potential callbacks.
Conclusion
Only 9% +/- 3% of our patients needed DCE to generate a PI-RADS version 2 score, raising the possibility of limiting the initial screening prostate MRI to an abbreviated non-contrast protocol.Acknowledgements
This work is supported by GE Healthcare.References
1. Weinreb JC, Barentsz JO, Choyke PL, et al. PI-RADS Prostate Imaging-Reporting and Data System: 2015, Version 2. Eur Urol 2016; 69: 16-40.
2. Greer MD, Shih JH, Lay N, et al. Validation of the dominant sequence paradigm and role of dynamic contrast-enhanced imaging in PI-RADS version 2. Radiology 2017; 286(1): 1-11.
3. Mussi TC, Martins T, Garcia RG, et al. Are Dynamic Contrast-Enhanced Images Necessary for Prostate Cancer Detection on Multiparametric Magnetic Resonance Imaging? Clinical Geniturinary Cancer 2017; 15(3): e447-e454.
4. De Visschere P, Lumen N, Ost P, et al. Dynamic contrast-enhanced imaging has limited added value over T2-weighted imaging and diffusion-weighted imaging when using PI-RADSv2 for diagnosis of clinically significant prostate cancer in patients with elevated PSA. Clinical Radiol 2017; 72: 23-32.
5. Le JD, Stephenson S, Brugger M, et al. Magnetic resonance imaging-ultrasound fusion biopsy for prediction of final prostate pathology. J Urol 2014; 192: 1367-1373.
6. Gupta RT, Spilseth B, Patel N, et al. Multiparametric prostate MRI: focus on T2-weighted imaging and role in staging of prostate cancer. Abdom Radiol 2016; 41: 831-843.
7. Flood TF, Pokharel SS, Patel NU, et al. Accuracy and interobserver variability in reporting of PI-RADS version 2. JACR 2017; 14(9): 1202-1205.
Figures