4369
Evaluation the Feasibility of Integrating Computer-aided Diagnosis as a Second Reader into Prostate Multiparametric MRI Diagnostic Process1Radiology, Peking University First Hospital, Beijing, China
Synopsis
Computer-aided diagnosis (CAD) for prostate cancer (PCa) detection based on multiparametric MRI (mpMRI) has become an active field of research, which has shown good stand-alone performance. Before its widely use in daily clinical work, further study still should be done for CAD reading paradigm and the interaction between CAD and human reader. In this article, we implemented CAD in the real world practice, aiming to evaluate the feasibility of integrating CAD as a second reader into the clinical diagnostic process. The results showed this reading paradigm was feasible and CAD might help readers detect more patients with PCa.
Introduction
The aim of this study is to evaluate the feasibility of integrating computer-aided
diagnosis (CAD) as a second reader into prostate multiparametric MRI (mpMRI) diagnostic
process in real clinical practice.
Methods
Eleven patients who had known prostate cancer were included. They undergone mpMRI (including T2WI, DWI and DCE) for the purpose of targeting the biopsy. Eighteen radiologists evaluated the cases, blinded to pathologic results. The prostate CAD results were reviewed during their image interpretation process, as following (Fig.1):
1. Readers interpreted mpMRI using structured report as routine clinical work, detected the lesions in the prostate gland, graded 1-5 points according to Prostate Imaging Reporting and Data System Version 2 (PI-RADS v2) and recorded diagnosis confidence with 1-5 points (1,absolutely not sure; 5, absolutely sure).
2. Readers recorded if they needed CAD for assisted diagnosis based on subjective needs. Regardless of what they chose, they needed to proceed to the next step.
3. With the assistance of CAD, readers could amend the scores they had made and then recorded diagnosis confidence again. Interpretation time was recorded by the system automatically.
Statistical Analysis: Patient was considered positive for PCa when at least one lesion was detected with a score of PIRADS 4 or 5. Diagnostic sensitivity with and without CAD was evaluated and compared using the McNemar test. Diagnostic confidence and interpretation time were evaluated and compared using Wilcoxon signed ranks test. The requirement for CAD was also evaluated.
Results
All the readers completed the entire diagnostic process smoothly. Diagnostic sensitivity and confidence were summarized in Table 1. With CAD assistance, the average diagnostic sensitivity was improved significantly(p<0.01). 11 readers performed better with CAD assistance and the sensitivity was improved from 54.5%-90.9% to 63.6% -100%. Diagnostic confidence of the readers was also improved significantly (p<0.001). All the readers’ average diagnostic confidence scores were higher with CAD.
Per lesion analysis was summarized in Table 2. CAD helped to detect some lesions that readers missed and improve the scores, especially for the lesions located in anterior fibromuscular stroma (AFS) (Fig.2) and apex with small size, 50.0%(9/18) and 22.2% (4/18) of the readers amended their scores upward respectively, followed by the transition zone (TZ) lesions. For the lesions with greatest dimension>1.0 cm located in peripheral zone (PZ), few readers amended their scores. Readers’ requirement rate of CAD varied for different lesions. For lesions located in AFS and apex, 94.4%(17/18) and 88.9%(16/18) of the readers chose CAD for further diagnosis,followed by TZ lesions. While the requirement rate of CAD was relatively low for PZ lesions. No readers amended their scores downward with CAD.
Furthermore, the average interpretation time of each case was 9.8 minutes without CAD, additional 0.7 minutes was required with CAD.
Discussion
Some studies demonstrated that CAD could support radiologists in differentiating pre-annotated benign lesions from malignant ones1-2. Giannini et al.3 compared the performance of experienced readers in detecting PCa using stand-alone CAD with that of unassisted mpMRI, which showed that the sensitivity increased in patients with prostate tumours≥10 mm and/or GS > 6. However, few studies evaluated CAD reading paradigm in real clinical practice. Our study simulated the daily radiological process and the results showed that CAD as a second reader could improve diagnostic sensitivity and confidence of the readers. Furthermore, the results indicated that CAD was useful for diagnosis of PCa located in AFS, apex with small size and TZ, which might be beneficial for directing prostate target biopsy. While CAD had little influence on the diagnosis of PCa located in PZ with the greatest dimension>1.0 cm. Therefore, personalized service of CAD to reduce the reading time may be a research direction in the future. Even though the reading time increased with CAD as a second reader, the additional 0.7 minutes was acceptable in clinical practice.Conclusion
It is feasible to integrate CAD as a second reader into prostate mpMRI diagnostic process. CAD may help radiologists detect PCa located in AFS, apex with small size and TZ.Acknowledgements
No acknowledgement found.References
1. Niaf E, Lartizien C, Bratan F, et al. Prostate focal peripheral zone lesions: characterization at multiparametric MR imaging--influence of a computer-aided diagnosis system. Radiology.2014; 271(3): 761-9.
2. Hambrock T, Vos PC, Hulsbergen-van de Kaa CA, et al. Prostate cancer: computer-aided diagnosis with multiparametric 3-T MR imaging--effect on observer performance. Radiology.2013; 266(2): 521-30.
3. Giannini V, Mazzetti S, Armando E, et al. Multiparametric magnetic resonance imaging of the prostate with computer-aided detection: experienced observer performance study. European radiology. 2017; 27(10): 4200–4208
Figures
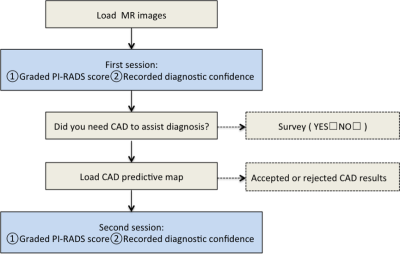
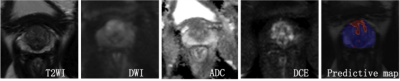
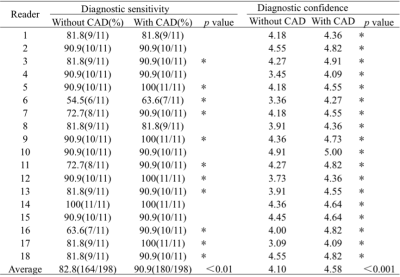
Table 1 Diagnostic sensitivity and diagnostic confidence of the 18 readers
* Diagnostic sensitivity and the scores of diagnostic confidence increased with CAD assistance
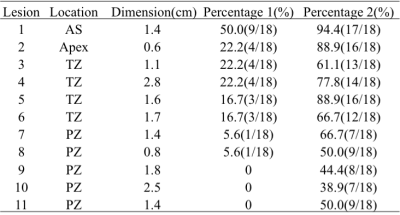
Table 2. Analysis of 11 PCa lesions
Percentage 1: the percentage of readers who amended the scores upward with CAD assistance
Percentage 2: the percentage of readers who chose CAD for further diagnosis in the survey