4365
MR imaging of the lung with a respiratory-gated ultrashort echo time (UTE) sequence with spiral acquisition technique: A feasibility study in oncology patients1Department of Radiology, Chung-Ang University Hospital, Seoul, Republic of Korea
Synopsis
We have demonstrated the feasibility of respiratory-gated ultrashort echo time sequence with spiral acquisition technique (spiral UTE; 1.5-mm isotropic resolution; echo time, 0.05 msec) of the lung for pulmonary nodule detection in oncology patients. Overall nodule detection rate was 86% (43 of 50 nodules) and the detection rate for nodules of ≥5 mm was 100 % (20 of 20 nodules). Mean acquisition time for spiral UTE was 327 seconds (range, 300 – 465 seconds). We think that spiral UTE could be a potential alternative to chest CT in oncology patients, who are in the risk of inevitable radiation exposure.
Introduction
Traditionally, computed tomography (CT) has been the modality of choice for most of the pulmonary disease. However, inevitable radiation exposure and its potential carcinogenic risks are major drawbacks of CT exams, especially for oncology patients who are in need of repeated imaging work up for the evaluation of tumor recurrence or metastasis. Meanwhile, with recent improvements in MR hardware and sequences, new techniques such as ultrashort echo time (UTE) have realized the clinical application of the MR imaging of the lung1-3. However, there are still well-known shortcomings of lung MR imaging such as long scan time, high expense, and unsatisfactory image quality4. In this study, we adopted spiral k-space trajectory, which is a promising option for rapid scan of UTE with preserved image quality due to its high readout efficiency and relatively insensitive motion effect5,6. We aimed to investigate the feasibility of respiratory-gated UTE sequence with spiral acquisition technique (spiral UTE) in oncology patients with extra focus on the semiquantitative image quality analysis and pulmonary nodule detection for metastasis work up.
Methods
Institutional review board approved this retrospective study with waiving of patient consent. Between June 2017 and September 2017, 32 oncology patients (13 hepatobiliary, 1 pancreatic, 1 gastric, 13 colorectal, 1 breast, 1 lung, 1 renal and 1 adrenal carcinomas) underwent both spiral UTE of the lung (1.5-mm isotropic resolution; echo time, 0.05 msec) and thin-section chest CT for pulmonary metastasis workup, with the Interval between the acquisition of MR and CT shorter than 30 days. Semiquantitative image quality analysis of spiral UTE was performed by two reviewers taking five aspects into consideration: (1) depiction of pulmonary vasculature, (2) depiction of airway, (3) image artifacts, (4) mediastinal evaluation, and (5) overall image quality. Presence of pulmonary nodules were also assessed on spiral UTE, using chest CT as a reference standard.Results
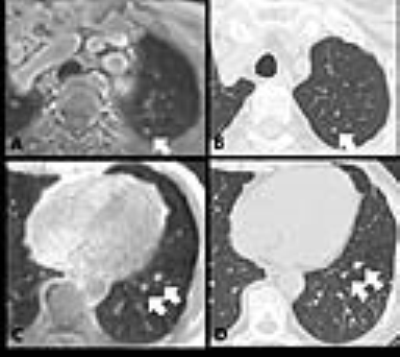
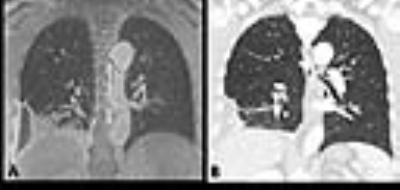
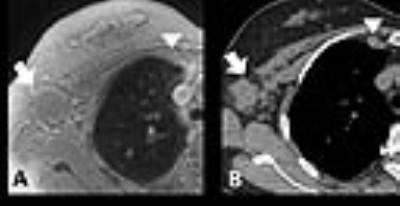
Mean acquisition time for spiral UTE was 327 seconds (range, 300 – 465 seconds). Pulmonary vessels and bronchi were visible nearly consistently up to the sub-sub-segmental (96.9%) and sub-segmental branch level (90.6%) on spiral UTE, respectively. Spiral UTE was assessed as acceptable or good for mediastinal evaluation in over 90% [R1 and R2; 96.9% (31 of 32) and 93.8% (30 of 32)]. In terms of image artifacts, reviewers evaluated that important or moderate artifacts were noted on 25% (8 of 32) and 28.1% (9 of 32) of spiral UTE images. However, overall image quality was rated as good or excellent in over 80% of spiral UTE [R1 and R2; 84.4% (27 of 32) and 81.3% (26 of 32)]. Interobserver agreements were moderate for mediastinal evaluation (k = 0.471), good for bronchial depiction, image artifacts, and overall image quality (k = 0.62, k = 0.775, and k = 0.699, respectively), and excellent for pulmonary vascular depiction (k = 1.00), respectively. Total 50 nodules (diameter, 6.1 ± 5.9 mm; range, 2.4 - 39 mm) were identified in 13 patients on CT and overall nodule detection rate of spiral UTE was 86% (43 of 50) (Figure 1). Twenty nodules, same or larger than 5 mm in diameter, were all identified on spiral UTE. Among seven nodules that were not detected on spiral UTE, six were located in the lung periphery and five were located in the lower lobes. Regarding other pulmonary and mediastinal findings, parenchymal consolidation (n = 2), pleural effusion (n = 2), micronodules with tree-in-bud appearance (n = 1), and lymph node enlargement (n = 2) were all well-identified on spiral UTE with 100% sensitivity (Figure 2 and 3). However, imaging of structural abnormalities such as bronchiectasis and pulmonary emphysema was still challenging, showing sensitivity of 40% and 33.3%, respectively.Discussion
We have demonstrated the feasibility of spiral UTE with 1.5-mm isotropic spatial resolution of the lung for the detection of pulmonary nodules in oncology patients. We think that the nodule detection rate and scan time of spiral UTE in our study was reasonable enough to be added as a part of the MR protocols using body coils such as the liver, pancreas, rectum or spine in oncology patients. Thus, we can evaluate the corresponding organs and lungs simultaneously, which enhances cost-effectiveness of MR study and patients’ convenience and decreases radiation exposure.Conclusion
A respiratory-gated spiral UTE has high sensitivity for the detection of pulmonary nodules with reasonable scan time and may be an alternative to CT in oncology patients.Acknowledgements
The authors thank the assistance of Siemens healthcare, which provided the ultrashort echo time sequence with spiral acquisition technique assessed in this study.References
1. Burris NS, Johnson KM, Larson PE, et al. Detection of Small Pulmonary Nodules with Ultrashort Echo Time Sequences in Oncology Patients by Using a PET/MR System. Radiology 2016;278:239-246.
2. Dournes G, Grodzki D, Macey J, et al. Quiet Submillimeter MR Imaging of the Lung Is Feasible with a PETRA Sequence at 1.5 T. Radiology 2015;276:258-265.
3. Ohno Y, Koyama H, Yoshikawa T, et al. Pulmonary high-resolution ultrashort TE MR imaging: Comparison with thin-section standard- and low-dose computed tomography for the assessment of pulmonary parenchyma diseases. Journal of magnetic resonance imaging : JMRI 2016;43:512-532.
4. Johnson KM, Fain SB, Schiebler ML, Nagle S. Optimized 3D ultrashort echo time pulmonary MRI. Magnetic resonance in medicine 2013;70:1241-1250.
5. Ahn CB, Kim JH, Cho ZH. High-speed spiral-scan echo planar NMR imaging-I. IEEE transactions on medical imaging 1986;5:2-7.
6. Kasper L, Engel M, Barmet C, et al. Rapid anatomical brain imaging using spiral acquisition and an expanded signal model. NeuroImage 2017.
Figures