4364
Pulmonary nodule detection using ultra-short TE (UTE) with a 3D variable-TE stack-of-spirals sequenceYu-Sen Huang1, Emi Niisato2, Mao-Yuan Marine Su1, Alto Stemmer3, Jin-Shing Chen4, and Yeun-Chung Chang1
1Department of Medical Imaging, National Taiwan University Hospital and National Taiwan University College of Medicine, Taipei, Taiwan, 2Siemens Healthcare Limited, Taipei, Taiwan, 3Siemens Healthcare GmbH, Erlangen, Germany, 4Department of Surgery, National Taiwan University Hospital and National Taiwan University College of Medicine, Taipei, Taiwan
Synopsis
UTE with 3D variable-TE stack-of-spirals sampling has been developed recently and allows shorter scan times by using undersampling in combination with an iterative, self-consistent parallel imaging reconstruction (SPIRiT). The goal of this study was to investigate the feasibility of this new technique in patients for detecting pulmonary nodules. The sequence was optimized for both free-breathing and breath-holding. Compared with CT images, the detection rate for pulmonary nodules in the UTE images was 92% for free-breathing and 75% for breath-holding. Our results suggest that the proposed UTE sequence has the capacity to detect pulmonary nodules under both free-breathing and breath-holding conditions.
Introduction
Lung MRI is a challenging task, given the low proton density, rapid signal decay, and B0 inhomogeneity. The UTE technique has emerged as a promising approach for lung MRI.1 For example, PETRA has been shown to be useful for the detection of lung nodules.2, 3 However, it resulted in long scan times because of its use of respiratory gating, preventing its wide clinical use. Another approach is 3D radial UTE sampling during breath-holding. However, the reported scan time was about 29 secs, which might be difficult for patients.4 Here, a 3D variable-TE UTE stack-of-spirals sequence5 (spiral UTE) is proposed for lung MRI to further improve the scan time. Two versions are presented: (i) data acquisition during free-breathing with self-navigation, and (ii) data acquisition during 20 secs of breath-holding for patients with an irregular breathing pattern. We aimed to show that the proposed spiral UTE sequence is capable of detecting pulmonary nodules.Methods
This study was approved by the Institutional Review Board of the hospital, and informed consent was obtained from all the enrolled participants. The images were acquired on a 1.5T scanner (MAGNETOM Aera, Siemens Healthcare, Erlangen, Germany). Thirteen control subjects and six patients with known lung nodules were enrolled by a chest surgeon. Two interpreting radiologists were blinded to the exact location of the lung nodules. A prototype spiral UTE was used for data acquisition as has been described in a previous study.5 The following parameters were used for the free-breathing protocol: TR/TE = 3.72 ms/0.05 ms, flip angle = 5°, spiral iPAT factor = 2, and voxel size = 1.56 x 1.56 x 1.56 mm3. For the breath-hold examination, the parameters were as follows: TR/TE = 3.34/0.05 ms, flip angle = 5°, spiral iPAT factor = 2, and voxel size = 2.08 x 2.08 x 2.1 mm3. The volumetric interpolated breath-holding examination (VIBE) sequence was used with a voxel size = 0.9 x 0.9 x 3.0 mm3. A lung CT was performed with a 128-slice CT scanner (Brilliance iCT, Philips Healthcare, Cleveland, OH, USA) with 120 kVp 119-235mA (modulated) and reconstructed coronally in 3 mm.Results
All the scans and reconstructions were performed successfully. Image quality of the spiral UTE was compared with the VIBE in the control subjects. Fig.1 shows the pulmonary branches are observed at a more peripheral distance using the spiral UTE approach compared with those in the VIBE images. The detection rate of the pulmonary nodules was analyzed in the patients' data. The free-breathing spiral UTE revealed a total of 11 nodules in 5 of the 6 patients (detection rate = 92%), and the breath-holding spiral UTE revealed a total of 9 nodules in 4 of the 6 patients (detection rate = 72%). CT identified 12 pulmonary nodules in 6 of the 6 patients (detection rate = 100%). There was no significant difference in the size of the nodules in the free-breathing spiral UTE (mean difference = 0.27 mm; 95% confidence interval (CI), 4.79 - 18.54 mm) and the breath-holding UTE (mean difference, 0.27 mm; 95% CI, 4.71 - 16.74 mm) compared to the CT images. Fig. 2 shows the comparison of the MR and CT images for a patient with a pulmonary nodule using the spiral UTE sequence.Discussion
Our pilot clinical trial showed that the spiral UTE sequence has a high nodule detection rate compared with CT. There was a 12-mm pure ground-glass nodule also clearly depicted by MRI and finally surgically proven to be a minimally invasive adenocarcinoma. However, the capacity of MRI to differentiate whether the lesion is solid or non-solid is still inferior to that of CT. In addition, we need to further validate the MRI performance, because we found one case in which a 12-mm non-solid nodule was undetectable by MRI near the pulmonary hilar region. The proposed spiral UTE sequence enables lung imaging with a high spatial resolution and short scan times. However, there are still some technical aspects that need to be improved upon. For example, the reconstruction time of the iterative reconstruction takes several minutes, which is longer than that of most clinical used sequences. Improvement of this reconstruction time will make it easier for radiologists to observe the data immediately after the scan has been completed.Conclusion
Our results demonstrated the potential use of the spiral UTE sequence. It detected the pulmonary nodules with an isotropic voxel size. The UTE sequence can not only be used under free-breathing conditions but also under breath-holding periods of 20 secs, which will be a realistic scan time for routine clinical work.Acknowledgements
This work was supported by the Ministry of Science and Technology, Taiwan (MOST 106-2221-E-002 -081 -MY3, NSC 102-2221-E-002 -029 -MY3 and NSC 100-2221-E-002 -031 -MY3)References
- Ohno Y, Koyama H, Matsumoto Y, et al. Lung MR imaging with ultra-short TE at 3.0T system: capability for pulmonary functional loss due to COPD. Proc. Intl. Soc. Mag. Reson. Med. 2010;18:203.
- Dornes G, Grodzki D, Macey J, et al. Quiet submillimeter MR imaging of the lung is feasible with a PETRA sequence at 1.5T. Radiology. 2015;276 (1):258-65.
- Natsuaki Y, Bi X, Laub G, and Grodzki D, et al. PETRA lung MRI: Towards robust lung imaging with patient comfort and with improved contrast. Proc. Intl. Soc. Mag. Reson. Med. 2016;24:2914.
- Herrmann KH, Krämer M, Reichenbach JR. Time efficient 3D radial UTE sampling with fully automatic delay compensation on a clinical 3T MR scanner. PLOS one. 2016;14:11(3).
- Fielden S, Mugler J, Miller W. et al. A variable-TE stack-of-spiral sequence for 3D UTE imaging. Proc. Intl. Soc. Mag. Reson. Med. 2016;24:1062. 6. Lustig M, and Pauly JM. SPIRiT: Iterative Self-consistent parallel imaging reconstruction form arbitrary k-space. Magn Reson Med. 2010;64(2):457-471.
Figures
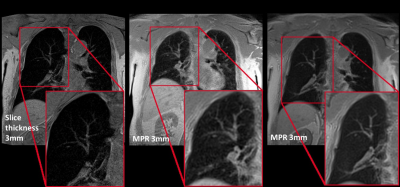
Lung branches were acquired with the VIBE sequence
during breath-holding and the spiral UTE sequences with free-breathing and
breath-holing. The branches can be observed at a more peripheral distance using
the spiral UTE approach. The VIBE image was acquired with a slice thickness of
3 mm. The spiral UTE images were acquired with a slice thickness of 1.56 mm.
For comparison, the spiral UTE images are depicted with an MPR thickness of 3
mm.
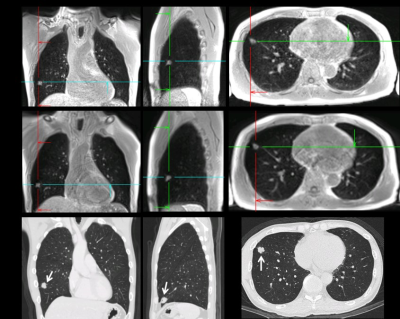
A solid nodule was detected with the spiral UTE
during both free-breathing and breath-holding. The images were acquired in the
coronal view, from which the sagittal and transverse images were obtained with
reformatting. The CT image shows a solid nodule (arrows), which correlates well
with the spiral UTE images.