4359
Multiparametric Approach by Quantitatively Assessed Dynamic First-Pass Contrast-Enhanced Perfusion MRI with FDG-PET/CT: Capability for Therapeutic Response Prediction in Non-Small Cell Lung Cancer After Conservative Therapy1Division of Functional and Diagnostic Imaging Research, Department of Radiology, Kobe University Graduate School of Medicine, Kobe, Japan, 2Advanced Biomedical Imaging Research Center, Kobe University Graduate School of Medicine, Kobe, Japan, 3Toshiba Medical Systems Corporation, Otawara, Japan, 4Division of Radiology, Department of Radiology, Kobe University Graduate School of Medicine, Kobe, Japan, 5Center for Radiology and Radiation Oncology, Kobe University Hospital, Kobe, Japan
Synopsis
To the best of our knowledge, no studies have been reported of a direct comparison of dynamic CE-perfusion MRI with PET/CT for therapeutic effect prediction for NSCLC patients treated with chemoradiotherapy. We hypothesized that multiparametric approach of quantitatively assessed dynamic CE-perfusion MRI with PET/CT have potential for better therapeutic effect prediction than single parametric methods by both modalities in NSCLC patients treated with chemoradiotherapy. The purpose of this study was therefore to directly compare the capability for therapeutic response prediction by among quantitatively assessed dynamic CE-perfusion MRI, FDG-PET/CT and multiparametric approach by both modalities in NSCLC patients treated with chemoradiotherapy.
Introduction
Since the early 2000s, several investigators have suggested that therapeutic effect prediction and/or assessment of non-small cell lung cancer (NSCLC) patients after conservative therapy could be performed with two dynamic imaging techniques, dynamic contrast-enhanced (CE) perfusion computed tomography (CT) and dynamic CE-magnetic resonance imaging (MRI) using the dynamic CE-perfusion MR method, and positron emission tomography (PET) or PET combined with CT (PET/CT) using 2-[fluorine-18]-fluoro-2-deoxy-D-glucose (FDG) and diffusion-weighted MR imaging (1-2). The results suggested that tumor perfusion parameters as well as glucose metabolism-based information are useful for therapeutic effect evaluation and/or prediction. To the best of our knowledge, however, no studies have been reported of a direct comparison of quantitatively assessed dynamic CE-perfusion MRI with PET/CT for therapeutic effect prediction for NSCLC patients treated with chemoradiotherapy. We hypothesized that quantitatively assessed multiparametric approach of quantitatively assessed dynamic CE-perfusion MRI with PET/CT have potential for better therapeutic effect prediction than single parametric methods by both modalities in NSCLC patients treated with chemoradiotherapy. The purpose of this study was therefore to directly compare the capability for therapeutic response prediction by among quantitatively assessed dynamic CE-perfusion MRI, FDG-PET/CT and multiparametric approach by both modalities in NSCLC patients treated with chemoradiotherapy.Methods and Materials
Forty three consecutive Stage IIIB NSCLC patients (25 men, 18 women; mean age 67 years) underwent PET/CT, dynamic CE-perfusion MRI, chemoradiotherapy, and follow-up examination. All dynamic CE-perfusion MRI using parallel imaging technique (TR 2.9 ms/ TE 1.1 ms/ flip angle 12 degree, reduction factor 2) were obtained at a 3T system (Vantage Titan 3T, Toshiba Medical Systems Corporation, Otawara, Japan), and all PET/CT examinations were performed by using standard technique on a PET/CT scanner (Discovery 600M, GE Healthcare, Waukesha, Wisc). In each patient, therapeutic outcomes were assessed as therapeutic effect based on RECIST guideline. Then, all patients were divided into two groups as follows: 1) responders (CR+PR cases: n=23) and 2) non-responders (SD+PD cases: n=20). In each patient, total perfusion (TP) and tumor perfusions from pulmonary (TPP) and systemic (TPS) circulations calculated from dynamic CE-perfusion MR data and SUVmax on PET/CT were assessed at each targeted lesion, and averaged to determine final values. All perfusion MR indexes were calculated by dual-input maximum slope methods. To determine each index difference between two groups, Student’s t-test was performed. Then, multivariate logistic regression analysis was performed to investigate the discriminating factors of responders. In addition, ROC analysis was performed to compare differentiating capability of responders from non-responders between multiparametric approach and each radiological index. Finally, sensitivity, specificity and accuracy were compared among all methods by McNemar’s test.Results
Representative case is shown in Figure 1. All indexes had significant differences between responders and non-responders (p<0.05). Multivariate regression analysis identified SUVmax (Odds ratio [OR]: 2.56) and TP (OR: 0.68) as significant differentiator of responder. Results of ROC analysis are shown in Figure 2. ROC analysis showed area under the curve (Az)of multiparametric approach (Az=0.95) was significantly larger than that of TPP (Az=0.72, p=0.001). Diagnostic performance of each method is shown in Figure 3. Sensitivity (95.7 [22/23] %) of multiparametric approach was significantly higher than that of TP (69.6 [16/23] %, p=0.03) and TPP (65.2 [15/23] %, p=0.02). Accuracy of multiparametric approach was significantly higher than that of TPP (p=0.004).Conclusion
Multiparametric approach of dynamic CE-perfusion MRI with PET/CT had better potential for therapeutic effect prediction than single parametric approach of dynamic CE-perfusion MRI and PET/CT in NSCLC patients treated with conservative therapy.Acknowledgements
This work was supported by Toshiba Medical Systems Corporation and Guerbet Japan.References
- Ohno Y, Nogami M, Higashino T, et al. J Magn Reson Imaging. 2005; 21: 775-783.
- Ohno Y, Koyama H, Yoshikawa T, et al. AJR Am J Roentgenol. 2012; 198: 75-82.
Figures
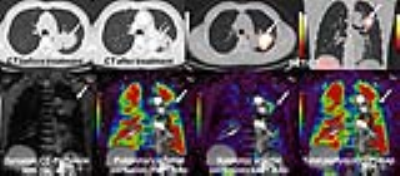
Figure 1. 68-year old female patient with adenocarcinoma treated by chemoradiotherapy and assessed the therapeutic effect as PR.
PET/CT demonstrates high uptake of FDG within tumor, and SUVmax was determined as 7.9. On quantitatively assessed dynamic CE-perfusion MRI, TP, TPP and TPS were determined as 91.2ml/100ml/min, 15.5ml/10mml/min and 75.7ml/100ml/min. Therefore, when feasible threshold values were applied, this case was responder case on SUVmax, TP and TPS, and non-responder case on TPP. In addition, when combined TP with SUVmax, this case was also determined as responder.

Figure 2. Results of ROC analysis among all indexes (left) and that of combined methods (right).
Area under the curve (Az) of combined method (Az=0.95) was significantly larger than that of TPP (Az=0.71, p=0.0001) and SUVmax (Az=0.78, p=0.03). In addition, Az of TP (Az=0.90) was significantly larger than that of TPP (p=0.0002).

Figure 3. Comparison of differentiation capability of responders from non-responders among all methods.
Sensitivity of multiparametric approach was significantly higher than that of TP (p=0.03) and TPP (p=0.02). Accuracy of multiparametric approach was significantly higher than that of TPP (p=0.004).