4348
Diffusion kurtosis imaging in solitary pulmonary nodules: comparison with quantitative dynamic contrast enhanced MR imaging in malignant and benign pulmonary nodule differentiationShuchang Zhou1, Liming Xia1, and Xu Yan2
1Radiology, Tongji Hospital of Huazhong University of Science and Technology, Wuhan, China, 2MR Collaboration NE Asia, Siemens Healthcare, Shanghai, China
Synopsis
Theoretically, DKI and quantitative DCE-MRI can provide more precise microstructure and perfusion information of tissues. However, the two methods had rarely been reported in solitary pulmonary nodules (SPNs) to date, so we collected 37 patients with SPNs underwent both DKI and DCE-MRI and measured relative parameters. The Kapp, Ktrans, Ve and iAUC values were significantly higher in lung cancer than in benignity. Kapp had best sensitivity and accuracy, and iAUC had best specificity. The combination of both methods can provide a robust way to discriminate SPNs before clinical management.
Introduction
Diffusion-weighted imaging (DWI) provides a promising method for characterizing pulmonary lesions to depict the water molecule diffusion further to mainly reflect the tissue cellularity [1]. Extended model such as IVIM is also considered as useful tool for further stratification of diffusion and perfusion of the tissues in pulmonary nodule differentiation[2, 3]. In fact, water diffusion of tissues in vivo has a non-Gaussian distribution due to the presence of diverse microstructures, so diffusion kurtosis imaging (DKI), [4-6]which quantifies non-Gaussian diffusion, is believed to better characterize tissue micro-structure than conventional DWI or IVIM model. Quantitative dynamic contrast enhanced MR imaging (DCE-MRI) is considered to be associated with vascular permeability and hence angiogenesis[3]. As more advanced functional MR tools, to our knowledge, the feasibility of the two methods were rarely reported and the comparison of the two methods in pulmonary nodule differentiation has not been established.Purpose
To evaluate the
feasibility of non-Gaussian model Diffusion kurtosis imaging (DKI) and quantitative
dynamic contrast enhanced MR imaging (DCE-MRI) in solitary pulmonary nodules
(SPNs) differentiation and compare the diagnostic value of both methods in
differentiating malignancies from benign SPNs.Materials and Methods
This study was approved by the local institute review
board, and written informed consent was obtained. Thirty-seven pathologically
confirmed SPNs in 37 consecutive patients were retrospective evaluated by DKI
using 5b-values (0, 400, 800, 1400 and 2000 s/mm2) and quantitative DCE-MRI on
3.0T MR. DKI (Kapp,Dapp) and DCE-MRI (Ktrans, Kep, Ve and iAUC), parameters
were measured and compared between lung cancer and benign nodules. Diagnostic performance
of these parameters was compared by ROC curves.Results
The Kapp, Ktrans, Ve and iAUC values in malignancies were significantly higher than those in benign SPNs (P=.018, P=0.034, P=0.034 and P=0.006, respectively).The diagnostic sensitivity and accuracy of Kapp value (81.8% and 75.7%) were higher than other indies (63.6%~72.7% and 70.3%~73.0%), The diagnostic specificity of iAUC value(80.0%) was higher than other parameters(66.7%~73.3%).The combination of Kapp and iAUC can improve the sensitivity, specificity and accuracy to 81.8%, 80% and 81.1%.Discussion
As previous study reported that kurtosis reflects the deviation of diffusion from Gaussian pattern [7],and can provide the microstructure complexity of tissue structure[8]. Diffusivity represents the diffusion with correction of non-Gaussian bias [7], thus equivalent to water molecule diffusion coefficient in mono-exponential DWI model. We found Kapp values were significantly higher in lung cancer than in benign nodules, while no significant difference was found for Dapp values. The results indicated that DKI can provide more precise characterization of tissue diverse microstructures such as cellular compartments and membranes, and may be a more promising way in differentiating the nuclear heterogeneity and complexity of tumor tissue profile. DCE-MRI based on a two-compartment (extended Tofts) model were applied in this study. We found that Ktrans,Ve and iAUC values were significantly higher in lung cancer compared to those in benignity. It indicated elevated perfusion and permeability of tumor microvessels and angiogenesis. Among these parameters, DKI derived Kapp had higher sensitivity and accuracy while iAUC had higher specificity. The combination of both metrics can provide a promising protocol for SPNs differentiation and can better demonstrate advanced characterization of tissue microstructure and perfusion.Conclusion
The initial results of this study confirmed the feasibility of DKI and quantitative DCE-MRI in lungs for assessment of malignant and benign SPNs. DKI showed higher sensitivity and accuracy than did DCE-MRI while DCE-MRI presented higher specificity for SPN differentiation. The combination of both methods can provide a more promising diagnosis of SPNs for clinical determination.Acknowledgements
No acknowledgement found.References
1. Broncano J, Luna A, Sanchez-Gonzalez J, et al. Functional MR Imaging in Chest Malignancies. Magn Reson Imaging Clin N Am. 2016;24(1):135-155. 2. Le BD, Breton E, Lallemand D, et al. Separation of diffusion and perfusion in intravoxel incoherent motion MR imaging. Radiology. 1988;168(2):497. 3. Yuan M, Zhang YD, Zhu C, et al. Comparison of intravoxel incoherent motion diffusion-weighted MR imaging with dynamic contrast-enhanced MRI for differentiating lung cancer from benign solitary pulmonary lesions. Journal of magnetic resonance imaging : JMRI. 2016;43(3):669-679. 4. Jensen JH, Helpern JA. MRI quantification of non-Gaussian water diffusion by kurtosis analysis. NMR in biomedicine. 2010;23(7):698-710. 5. Le Bihan D. Molecular diffusion, tissue microdynamics and microstructure. NMR in biomedicine. 1995;8(7-8):375-386. 6. Rosenkrantz AB, Padhani AR, Chenevert TL, et al. Body diffusion kurtosis imaging: Basic principles, applications, and considerations for clinical practice. Journal of magnetic resonance imaging : JMRI. 2015;42(5):1190-1202. 7. Rosenkrantz AB, Sigmund EE, Johnson G, et al. Prostate cancer: feasibility and preliminary experience of a diffusional kurtosis model for detection and assessment of aggressiveness of peripheral zone cancer. Radiology. 2012;264(1):126-135. 8. Jensen JH, Helpern JA, Ramani A, et al. Diffusional kurtosis imaging: the quantification of non-gaussian water diffusion by means of magnetic resonance imaging. Magnetic resonance in medicine. 2005;53(6):1432-1440.Figures
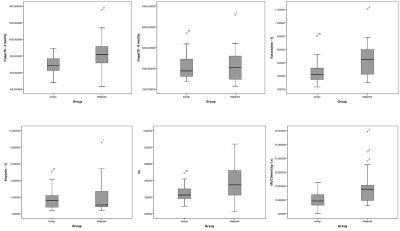
Box plots of
Kapp, Dapp, Ktrans, Kep, Ve and iAUC values in LC and benign lesions. Top
and bottom lines are 25 and 75 percentiles of the data, respectively. Line
in the middle represents median value. LC showed significantly higher
Kapp, Ktrans, Ve and iAUC values(P≤0.05). Dapp showed no significant
difference.
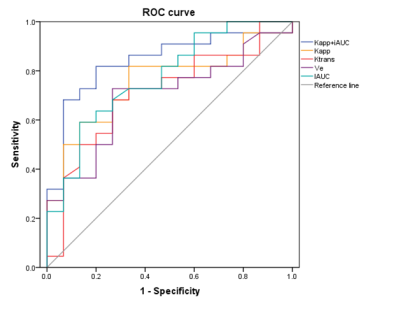
ROC curves of Kapp, Ktrans, Ve , iAUC, combined
Kapp and iAUC for discriminating benign from malignant SPNs. Kapp and iAUC had larger
AUC, Kapp had the highest sensitivity and accuracy, and iAUC had the highest
specificity.
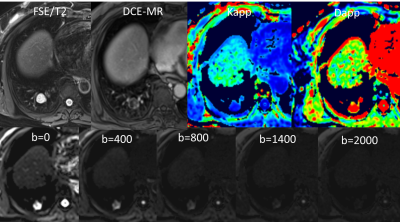
A chondroma of
right lower lobe in a 62-year-old female. FSE/T2, DCE-MR (a phase), Kapp, Dapp and
multi-b value images. In this case, T2 showed a mixed long T2 signal, DCE-MRI
showed an annular enhancement with nodular enhancement, Kapp= 479× 10–3 mm2/s, Dapp =2.92× 10–3 mm2/s. With the increase of b value, SI decreased
gradually.