4346
Functional lung imaging with partially spoiled ultra-fast steady-state free precession at 1.5T and 3T1Division of Radiological Physics, Department of Radiology, University of Basel Hospital, Basel, Switzerland, 2Department of Biomedical Engineering, University of Basel, Basel, Switzerland
Synopsis
In this work we propose an alternative acquisition framework for functional lung imaging using matrix pencil (MP) decomposition (a derivative of Fourier decomposition method) based on partially spoiled ultra-fast steady-state free-precession (ps-ufSSFP) imaging. We showed that MP decomposition is feasible in healthy volunteers using ps-ufSSFP at 1.5T and 3T. Hence, ps-ufSSFP can be a viable solution for the application of MP MRI at 3T where imaging with balanced ufSSFP can be problematic due to the occurrence of off-resonance artifacts.
Purpose
Functional lung MRI using matrix pencil decomposition (MP)1 or Fourier decomposition (FD)2 technique relies on dynamic free-breathing acquisitions of native chest images. The acquired time-resolved data sets are used for the calculation of functional lung images including fractional ventilation, relative perfusion or blood arrival time maps.1Despite the approach has already shown promise for clinical use,3-5 its application using the balanced steady-state free precession imaging at 3T is still limited by off-resonances resulting in non-diagnostic image quality. Currently, it is also the main limiting factor for the adoption of MP MRI in centers with access to only 3T scanners. To this end, we implemented a partially-spoiled ultra-fast gradient echo pulse (ps-ufSSFP) sequence by substantial reduction of TE/TR and adapted acquisition scheme for improved dynamic lung imaging. The purpose of this work was to test the proposed acquisition approach as a possible framework for MP MRI in healthy volunteers at 1.5T and 3T.
Methods
MR data acquisition
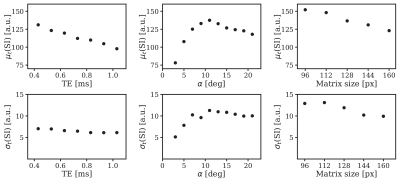
Measurements were performed on 1.5T (Avanto-Fit, Siemens Healthineers, Germany) and 3T (Prisma, Siemens Healthineers, Germany) MR scanners using a combination on thorax and spine receiver coils. Three healthy volunteers were scanned in free-breathing with the adapted ps-ufSSFP sequence at 1.5T and 3T as well as with ultra-fast steady-state free precession (ufSSFP) sequence for reference at 1.5T. For the optimization of the ps-ufSSFP sequence, relations between the signal intensity (SI) in the lung tissue and the flip angle α, TE, TR length, matrix size were studied. Scans were performed with variable TE = 0.43 - 1.03 ms, TR = 0.99 - 3.99 ms, α = 3 - 21°, matrix size = 96x96 - 160x160, standard 50° RF spoiling, partial RF spoiling of 5°, as well as linear or centric reordering.
Parameters kept constant in all scans were: acquisition rate = 3.33 images/s, GRAPPA factor 2, slice thickness = 12 mm, field-of-view = 450x450 mm2, data set length of 160 images per slice. Acquisitions with balanced ufSSFP were performed at 1.5T with TE/TR = 0.67/1.45 ms, TW = 180 ms, α = 65°, matrix=128x128.
Image postprocessing and analysis
Time-resolved data sets were processed using non-rigid image registration and matrix pencil decomposition to generate fractional ventilation, relative perfusion and blood arrival time images. Signal intensity (SI) and signal-to-noise ratio (SNR) in the segmented lung area was analyzed in every registered time-resolved data set as well as from the baseline signal component of the matrix pencil decomposition. A set of ps-ufSSFP parameters providing the highest SI in the lung was identified and used to define protocols for 1.5T and 3T.
Results
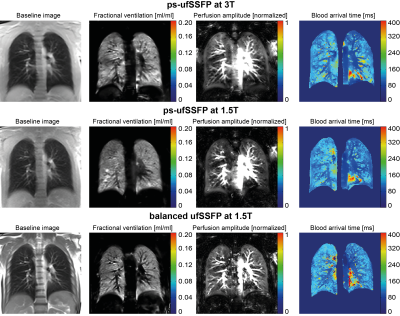
Mean and standard deviation of the signal in the lung parenchyma as a function of TE, α and matrix size is shown in Figure 1. Generally SI decreases with increasing TE and matrix size. The optimal flip angle was around 11° for 1.5T and 9° for 3T. Partially spoiled acquisitions provided 9.6% higher SI than fully spoiled. Acquisitions performed with the shortest TR of 0.99 ms yielded the highest SI in the lung due to the transient nature of the signal. Average SNR in the lung was 73.3±16.7 for balanced ufSSFP, 38.1±13.3 for ps-ufSSFP at 1.5T, and 35.6±12.8 for ps-ufSSFP at 3T. Figure 2 shows exemplary native images, fractional ventilation and relative perfusion maps acquired using balanced ufSSFP and ps-ufSSFP at 1.5T and 3T.Discussion and Conclusion
In this work we propose an alternative acquisition framework for functional lung imaging using matrix pencil decomposition based on ps-ufSSFP. The presented acquisition scheme uses partial RF spoiling combined with sub-millisecond repetition time and centric readout of the transient signal. For the standard matrix size of 128x128, the TE/TR of ps-ufSSFP were 0.43/0.99ms at both field strengths. ps-ufSSFP acquisition allows for generation of functional lung maps in healthy volunteers at 1.5T and 3T. Although ps-ufSSFP does not achieve SNR of balanced ufSSFP in the lung tissue at 1.5T, ps-ufSSFP can be a viable solution for the implementation of MP MRI at 3T where the application of balanced ufSSFP is currently not feasible. However, further studies are required to test whether functional impairment can be successfully detected using the proposed imaging technique.
Acknowledgements
Siemens Healthineers for providing image registration software.References
1. Bauman G, Pusterla O, Bieri O. Ultra-fast steady-state free precessionpulse sequence for Fourier decomposition pulmonary MRI. Magn Reson Med 2016;75:1647–1653.
2. Bauman G, Bieri O. Matrix pencil decomposition of time-resolved proton MRI forrobust and improved assessment of pulmonary ventilation and perfusion. Magn Reson Med. 2017 Jan;77(1):336-342.
3. Sommer G, Bauman G, Koenigkam-Santos M, et al. Non-contrast-enhanced preoperative assessment of lung perfusion in patients with non-small-cell lung cancer using Fourier decompositionmagnetic resonance imaging. Eur J Radiol. 2013 Dec;82(12):e879-87.
4. Schönfeld C, Cebotari S, Voskrebenzev A, et al. Performance ofperfusion-weighted Fourier decomposition MRI for detection of chronic pulmonaryemboli. J Magn Reson Imaging. 2015 Jul;42(1):72-9.
5. Capaldi DP, Sheikh K, Guo F, et al. Free-breathing pulmonary 1H and Hyperpolarized 3HeMRI: comparison in COPD and bronchiectasis. Acad Radiol. 2015 Mar;22(3):320-9.
Figures