4330
Quality assessment with a breast phantom and a volunteer for multi-institutional MRI trials including DWI1Department of Diagnostic Imaging and Nuclear Medicine, Graduate School of Medicine, Kyoto University, Kyoto, Japan, 2Hakubi Center for Advanced Research, Kyoto University, Kyoto, Japan, 3Siemens Healthcare K.K., Tokyo, Japan, 4Kitano Hospital, The Tauke Kofukai Medical Research Institute, Osaka, Japan, 5Kurashiki Central Hospital, Kurashiki, Japan, 6Shiga hospital, Japan Community Health care Organization, Otsu, Japan, 7Philips Japan, Tokyo, Japan
Synopsis
The novel method for quality control applicable for commonly used breast MR images (T1WI, T2WI and DWI) in terms of semi-quantitative and quantitative analysis was proposed. The scan was performed across multiple sites on both a breast phantom and a volunteer. The provided scores and apparent spatial resolution were comparable between a phantom and a volunteer. Quality of breast MR images across sites were variable, and standardization using a dedicated breast phantom is considered necessary to assure good diagnostic performance of breast MRI.
Introduction
Breast MRI has been increasingly used in the screening of high risk women or for treatment monitoring1, with a special emphasis on diffusion MRI for the characterization of breast tumors without the need for contrast agents.2 However, results, expressed as ADC values, are highly variable across the literature. Hence, for diffusion MRI to be used in clinical setting or within multicenter trial,3 quality control assessment and standardization of breast MRI protocols is a paramount issue.4 Quality control in T1WI, T2WI5 or DWI6 has been reported, however, the assessment incorporating T1WI, T2WI and DWI, all of which are commonly used in clinical setting, and using both a breast phantom and a volunteer have rarely been investigated. Here, we propose to go one step further by assessing the quality of T1WI, T2WI and DWI in terms of semi-quantitative and quantitative analysis from images acquired across multiple sites using both a breast phantom and a volunteer.Methods
A bilateral breast phantom was developed; one side contained a plate with multiple widths of slits (8 slits each for 0.5, 0.6, 0.8, 1, 2 and 3mm widths) for the estimation of spatial resolution, and the other side incorporated compartment with a range of ADC values (using polyvinylpyrrolidone (PVP) and nonane), covering clinical values from malignant to benign lesions6 (Fig.1). T1W, T2W and DW images of the breast phantom and a volunteer were acquired across 4 centers (two scanners each for 3T and 1.5T; detailed acquisition protocols shown in Table 1, with room temperature at 25℃). T1W and T2W images with high resolution were also acquired to generate the “reference” images to directly compare the images across multiple sites. “Apparent spatial resolution” at each site was inferred by following steps; sample images of a normal volunteer were scanned with 0.5mm in-plane resolution (total acquisition time (TA) ~8min), which was much higher than in clinical setting (TA~2.5min). Reference image sets were calculated by applying rectangular window filter in k-space of the sample images corresponding to 0.5~2.0mm (0.1mm step) spatial resolution using matlab (Mathwork, Natick, MA). Two breast radiologists assigned “apparent spatial resolution” to volunteer images at each site by comparing the reference image sets (regarding contour of breast etc) on consensus.
Semi- quantitative analysis: T1W, T2W and DW images in a phantom and normal breasts were read by two independent breast radiologists and 0-4 scores were assigned to evaluate image quality for each site (Fig.1), and their agreement was evaluated using weighted kappa.
Quantitative analysis: ADC values (obtained using b=0 and 600s/mm2) were calculated using ROIs in the compartments containing different PVP solutions and nonane for each DWI dataset.
Results
The representative images of a breast phantom along the equivalent apparent resolution for all sites are shown in Fig.2-3. The equivalent apparent resolution varied more in T1W compared to T2W images. The apparent resolution seems not so different from their real MR images.
The result of scores is summarized in Fig.4. The scores from 2 readers for each site was averaged due to good agreement (weighted Kappa: 0.95-0.975). The scores for 4 sites became variable with 0.8-1.0mm slit for both T1W and T2W images. The appreciation of 3mm slit was most variable across 4 sites for DW images. All breast MR images of a volunteer varied across scanners, however, the scores obtained from a phantom and a volunteer as well as apparent resolutions were comparable at each site.
Discussion
We have shown the preliminary result of quality control for the commonly-used breast MR images, and the results obtained from a phantom and a volunteer using semi-quantitative and quantitative analysis were comparable at each site. The slit with 0.8-1.0mm for T1W and T2W images was variably scored across sites. This indicates that sub-millimeter feature could be differently appreciated, which could influence the findings of spiculation, etc. The distributions of scales with 3mm slit on breast DW images indicated small lesions could be missed, still the limitation in the clinical setting, especially for differentiating small lesions from normal tissue . On the other hand relatively small lesions could often be easily detected on the DW images even with low SNR, although the structure of normal breast issue can be hardly appreciated on DW images. Hence, the apparent resolution using phantoms are considered as necessary for the direct comparison of breast MR images across different sites, or regular maintenance of the MRI scanner.Conclusion
We proposed the novel method for quality control applicable for all breast MR images, which can provide objective assessments of both phantom and volunteer images. Quality of breast MR images across sites were variable, and standardization using breast phantoms is recommended to assure good diagnostic performance of breast MRI.
Acknowledgements
This work was supported by Hakubi Project of Kyoto University and MEXT KAKENHI Grant No. 15K19786.References
1. American College of Radiology. (2016). ACR practice parameter for the performance of contrast-enhanced magnetic resonance imaging (MRI) or the breast. Updated 2013.
2. Partridge SC, Nissan N, Rahbar H, et al. Diffusion-weighted breast MRI: Clinical applications and emerging techniques. J Magn Reson Imaging. 2017;45(2):337-355.
3. Malyarenko D, Galbán CJ, Londy FJ, et al. Multi-system repeatability and reproducibility of apparent diffusion coefficient measurement using an ice-water phantom. J Magn Reson Imaging. 2013; 37(5): 1238–1246.
4. Kinetic Curves of Malignant Lesions Are Not Consistent Across MRI Systems: Need for Improved Standardization of Breast Dynamic Contrast-Enhanced MRI Acquisition. AJR Am J Roentgenol. 2009; 193(3): 832–839.
5. Tuong B, Gardiner I. Development of a novel breast MRI phantom for quality control. AJR Am J Roentgenol. 2013;201(3):W511-5
6. Keenan KE, Peskin AP, Wilmes LJ, et al. Variability and bias assessment in breast ADC measuremnt across multiple systems. J Magn Reson Imaging. 2016 ;44(4):846-55.
Figures
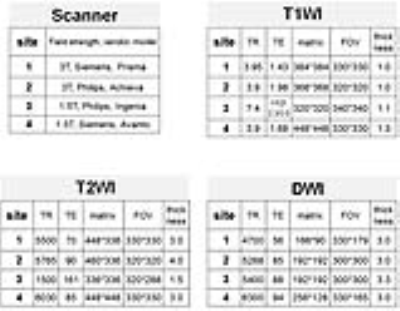


Figure 2: The representative T1-weighted images of a breast phantom and a volunteer for 4 sites.
The equivalent apparent resolution of each breast image is also shown in the upper left corner of the breast images.

Figure 3: The representative T2-weighted images of a breast phantom and a volunteer with the equivalent apparent resolution for 4 sites.
The equivalent apparent resolution of each breast image is also shown in the upper left corner of the breast images.

Figure 4: Box-whisker plots of the scores and ADC values for a phantom, and the scores for a volunteer.
T1WI, T2WI and DWI scores at each slit width are provided for a phantom. ADC values were measured in 10%, 14%, 18%, 25% and 40% PVP, water and nonane of a phantom. T1WI, T2WI and DWI scores for each breast image is shown for a volunteer.