4197
Dentate Nucleus Signal Intensity Decrease on T1-Weighted MR Images after Switching from Linear to Macrocyclic GBCA1Radiology, Weill Cornell University, New York, NY, United States, 2Weill Cornell University, New York, NY, United States, 3Radiology, weill Cornell Medical College, New York, NY, United States
Synopsis
Dentate Nucleus signal intensity ratios decreased with time after switching from linear (gadopentetate) to macrocyclic (gadobutrol) agent.
Purpose: The purpose of this study was to determine if the increased Dentate Nucleus signal intensity following 6 or more linear GBCA, gadopentetate dimeglumine, administrations changes on follow-up exams using exclusively macrocyclic GBCA, gadobutrol.
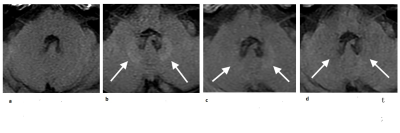
Methods: This retrospective study included 13 patients with increased dentate nucleus signal following ≥ 6 (6-18) linear GBCA administrations who then had at least 12 months follow-up imaging with multiple (3-29) macrocyclic only GBCA enhanced MRI exams. Dentate nucleus to pons (DNP) and to cerebellar peduncle (DNCP) signal intensity ratios were measured by 2 blinded radiologists and the changes were analyzed using paired t test and mixed effect model regression.
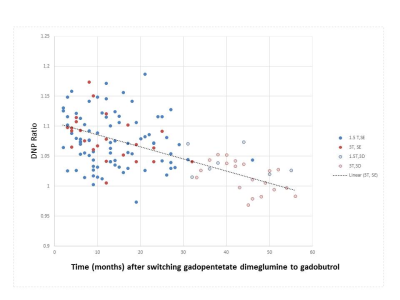
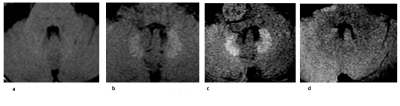
Results: Results: Mean DNP and DNCP increased following gadopentetate dimeglumine from 0.979 ± 0.026 to 1.103±0.030 (p<0.0001), and 0.977 ±0.030 to 1.093 ±0.025 (p<0.0001) respectively . After switching to using gadobutrol the DNP and DNCP signal intensity ratios decreased to 1.027 ± 0.033and 1.023 ± 0.036 (p<0.0001). Linear regression using a mixed effects model allowing for each patient to have a different y intercept showed DNP and DNCP decreased with follow up time (p<0.0001; slope = -0.2 %/month ;( 95% CI: -0.0021, -0.0012; R2=0.58), and slope=-0.2 %/month (95% CI: -0.0020, -0.0011; R2=0.61) respectively (p<0.000001 for non-zero slope)
Conclusion: Dentate signal intensity increases with ≥ 6 linear GBCA enhanced MRI exams, decreased after switching from linear (gadopentetate dimeglumine) to macrocyclic (gadobutrol) GBCA.
Acknowledgements
No acknowledgement found.References
1. Smith AP, Marino M, Roberts J, et al. Clearance of Gadolinium from the Brain with No Pathologic Effect after Repeated Administration of Gadodiamide in Healthy Rats: An Analytical and Histologic Study. Radiology. 2017; 282(3):743-751
3. Robert P, Violas X, Grand S, et al. Linear gadolinium-based contrast agents are associated with brain gadolinium retention in healthy rats. Invest Radiol 2016; 51(2):73–82.
4. McDonald RJ, McDonald JS, Dai D, Schroeder D, Jentoft ME, Murray DL, Kadirvel R, Eckel LJ, Kallmes DF. Comparison of Gadolinium Concentrations within Multiple Rat Organs after Intravenous Administration of Linear versus Macrocyclic Gadolinium Chelates. Radiology. 2017 Jun 19:161594.
5. Kanal E, Tweedle MF. Residual or retained gadolinium: practical implications for radiologists and our patients. Radiology. 2015; 275:634–630.
6. Prybylski JP, Maxwell E, Coste Sanchez C, Jay M. Gadolinium deposition in the brain: Lessons learned from other metals known to cross the blood-brain barrier. Magn Reson Imaging. 2016; 34(10):1366-1372.
8. Frenzel T, Apte C, Jost G, Schöckel L, Lohrke J, Pietsch H. Quantification and Assessment of the Chemical Form of Residual Gadolinium in the Brain After Repeated Administration of Gadolinium-Based Contrast Agents: Comparative Study in Rats. Invest Radiol. 2017 Jul; 52(7):396-404.
Figures