4192
Absence of T1 hyperintensity in the brain of high-risk iron loaded thalassemia patients after multiple administrations of high dose Gadobutrol1Fondazione G. Monasterio CNR-Regione Toscana, Pisa, Italy, 2Policlinico Università di Bari, Bari, Italy, 3Azienda Ospedaliera di Rilievo Nazionale "A. Cardarelli", Napoli, Italy, 4Ospedale “Meyer”, Firenze, Italy, 5Ospedale "San Donato", Arezzo, Italy
Synopsis
Our study describes the lack of increased signal intensity (SI) in T1-weighted MRI images after repeated administrations of Gadobutrol in a high-risk population (high dose/scan, iron overload that facilitates the transmetallation of gadolinium). A potential role of the chelation therapy cannot be excluded. Moreover, it is highlighted that SI ratios in the sampled areas differ between 1.5T and 3T.
Introduction
Late gadolinium enhancement (LGE) cardiovascular magnetic resonance (CMR) is a unique non-invasive technique validated to detect necrosis/fibrosis1. However, many studies have reported an association between increased signal intensities (SI) on unenhanced T1-weighted MR images in different brain regions and the history of repeated intravenous administrations of Gadolinium based contrast agents (GBCA) in patients with normal renal function2-6.
We conducted a prospective study aimed to evaluate signal changes in the dentate nucleus (DN), globus pallidus (GP), pons, and thalamus (normalized to the deep cerebellum white matter) in T1-MRI images after serial injections of Gadobutrol for the LGE-CMR in patients with thalassemia.
Methods
Among the thalassemic patients who underwent a brain MRI within a pilot study for iron overload assessment, we selected two groups of patients: 15 patients transfused and chelated with≥4 Gadobutrol administrations at a high dose (0.2 mmol/Kg per scan), 8 thalassemia patients who never received Gadobutrol. Moreover, we included 13 healthy subjects who never received Gadobutrol as control group.
All three groups were scanned at 1.5T and 3T.
Iron overload was assessed by the T2* technique.
Results
Mean age and proportion of females were comparable among the three groups.
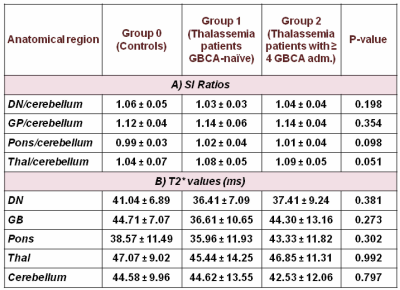
All SI ratios obtained at 1.5T are shown in Table 1A. No significant differences were obtained among the three groups. As shown in Table 1B, the T2* values in all regions were comparable among the three groups. Moreover, no correlation was detected between SI ratios and T2* values.
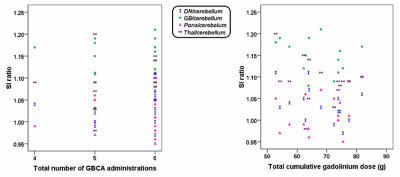
We selected only the patients with more than 4 GBCA administrations. The SI ratios were analyzed relative to the total cumulative gadolinium dose and total number of contrast-enhanced examinations (Figure 1) and no association was detected.
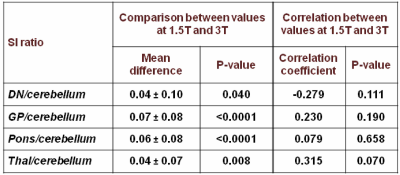
The signal of all brain regions was significantly lower at 1.5 T than at 3T. However, for all the sampled brain regions the SI ratios at 1.5T were significantly higher than those obtained at 3T. Moreover, no correlation was found between SI ratios at 1.5T and 3T (Table 2).
Conclusion
It is important to underline that thalassemia patients represent an high-risk population for the GBCA accumulation, due to the fact that, in presence of siderosis, ferric ions can compete with Gadolinium ions for the ligand, destabilizing the gadolinium complex. Nevertheless, our study describes the lack of increased SI after repeated administration of Gadobutrol, a nonionic macrocyclic agent.
All our patients were chelated when they received the GBCA. Different studies showed the ability of all three iron chelators to chelate other metals7,8. So, a potential role of chelation therapy may be supposed.
Moreover, it is highlighted that SI ratios in the sampled areas differ between 1.5T and 3T.
Acknowledgements
No acknowledgement found.References
1. Mahrholdt H, Wagner A, Judd RM, Sechtem U, Kim RJ. Delayed enhancement cardiovascular magnetic resonance assessment of non-ischaemic cardiomyopathies. Eur Heart J 2005;26(15):1461-1474.
2. Kanda T, Ishii K, Kawaguchi H, Kitajima K, Takenaka D. High signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted MR images: relationship with increasing cumulative dose of a gadolinium-based contrast material. Radiology 2014;270(3):834-841.
3. Errante Y, Cirimele V, Mallio CA, Di Lazzaro V, Zobel BB, Quattrocchi CC. Progressive increase of T1 signal intensity of the dentate nucleus on unenhanced magnetic resonance images is associated with cumulative doses of intravenously administered gadodiamide in patients with normal renal function, suggesting dechelation. Invest Radiol 2014;49(10):685-690.
4. Quattrocchi CC, Mallio CA, Errante Y, et al. Gadodiamide and Dentate Nucleus T1 Hyperintensity in Patients With Meningioma Evaluated by Multiple Follow-Up Contrast-Enhanced Magnetic Resonance Examinations With No Systemic Interval Therapy. Invest Radiol 2015;50(7):470-472.
5. Radbruch A, Weberling LD, Kieslich PJ, et al. Gadolinium retention in the dentate nucleus and globus pallidus is dependent on the class of contrast agent. Radiology 2015;275(3):783-791.
6. Adin ME, Kleinberg L, Vaidya D, Zan E, Mirbagheri S, Yousem DM. Hyperintense Dentate Nuclei on T1-Weighted MRI: Relation to Repeat Gadolinium Administration. AJNR Am J Neuroradiol 2015;36(10):1859-1865.
7. Douthat WG, Acuna Aguerre G, Fernandez Martin JL, Mouzo R, Cannata Andia JB. Treatment of aluminium intoxication: a new scheme for desferrioxamine administration. Nephrol Dial Transplant 1994;9(10):1431-1434.
8. Fatemi SJ, Khajoee nejad F, Zandevakili T, Dahoee balooch F. Chelation of cobalt by combining deferasirox, deferiprone and desferrioxamine in rats. Toxin Reviews 2013;33(4):146-150.